
- Hearing loss in Adults
- Tinnitus
- Noise induced Hearing loss
- Hearing loss in Children
- Otitis Media with Effusion (OME)
- ASOM (Acute Suppurative Otitis Media)
- Chronic Suppurative Otitis Media
- Otitis Externa (Outer ear infection)
- Ear Wax
- Otomycosis (Fungal infection of the ear)
- Otosclerosis (Fixation of the bones of hearing)
- Giddiness due to Benign paroxysmal positional vertigo (BPPV)
How can I tell if I have a hearing loss?
If you answer yes to some of the following questions, you may have a hearing loss
Often ask people to repeat what they say?
Have trouble hearing in groups?
Think others mumble?
Turn up the volume on the TV or car radio?
Have difficulty on the phone?
Have trouble hearing your alarm clock?
Have difficulty hearing at the movies?
Dread going to noisy parties and restaurants?
Think about these situations
Are you embarrassed to talk openly about not being able to hear?
Are you cutting out activities that you used to love but have become painful because you cannot join in fully anymore?
At work are you afraid to reveal your hearing loss in case it jeopardizes your job and your supervisor and co-workers may see you as less competent?
Are you bluffing when out with friends in noisy restaurants?
Are you feeling cut off from your young children because you cannot hear their high-pitched voices?
Are family holidays a strain because so many people are talking at once?
These are common reactions and can lead to withdrawal from social interaction, anxiety, loss of self-esteem and even depression.
Do You Know Someone Who May Not Admit He or She Has a Hearing Loss?
If you think, you or someone you know might have a hearing loss, you are not alone. If you have suspected for a while but just haven’t got around to doing anything about it, that is not unusual.
“I can hear but can’t understand.”
For most adults, the onset and progression of a hearing loss extends over some time. Often, people will blame their hearing problems on the nature of the other person’s speech. For example, someone might say: “If people wouldn’t mumble, I could hear! “Or, “People talked a lot clearer when I was younger.” One’s family and friends are likely to be the first to notice some difficulty hearing, long before the person does. Typically at this stage, the individual will deny a problem. This is understandable, since there is usually great variability in how the person functions in various situations and with different people. In some situations and with some people, he or she may do pretty well. People will not be aware of what they don’t hear (like the sounds of birds, the beep of the microwave, and soft everyday sounds). They will be aware that they do not understand speech, as when they say, “I can hear but can’t understand,” especially the high-pitched voices of children.
Family members frequently complain that the TV volume is set too high, leading to some family squabbles. The person with hearing loss will notice difficulty in understanding when someone talks from another room. Probably, the major complaint of people with hearing loss is the difficulty they experience in comprehending speech in any kind of noisy place (restaurants, receptions, large family dinners, in the car, or on a plane).
Group conversations are particularly difficult, especially when there is great deal of cross-talk.
These increasing difficulties in hearing may produce conflict between the person with hearing loss and family members, with the family insisting on getting help and the person with hearing loss reluctant to recognize the reality. For children who are hard of hearing, the situation is different. Parents should be on the lookout for delayed or aberrant speech and language development, apparent inattention, and poor school work. Hearing loss can be caused by many different causes, some of which can be successfully treated with medicine or surgery, depending on the disease process.
Three Types of Hearing Loss
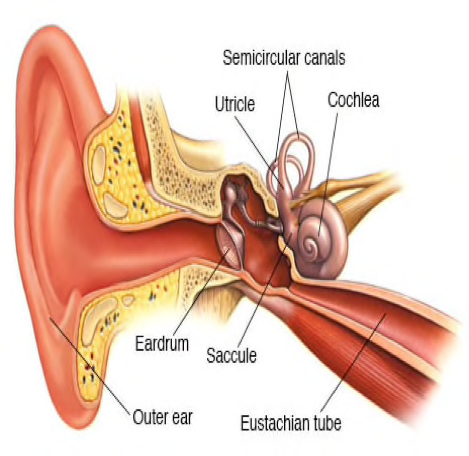
Conductive hearing loss
When hearing, loss is due to problems with the ear canal, ear drum, or middle ear and its little bones (the malleus, incus, and stapes).
Causes:
- Malformation of outer ear, ear canal, or middle ear structures
- Fluid in the middle ear from colds
- Ear infection (otitis media – an infection of the middle ear in which an accumulation of fluid may interfere with the movement of the eardrum and ossicles)
- Allergies
- Poor Eustachian tube function
- Perforated eardrum
- Benign tumors
- Impacted earwax
- Infection in the ear canal
- Foreign body in the ear
- Otosclerosis
Treatments of Conductive Hearing Loss:
Types of conductive hearing loss include congenital absence of ear canal or failure of the ear canal to be open at birth, congenital absence, malformation, or dysfunction of the middle ear structures, all of which may possibly be surgically corrected. If these are not amenable to successful surgical correction, then the hearing alternatively may be improved with amplification with a bone conduction hearing aid, or a surgically implanted, osseointegrated device, or a conventional hearing aid, depending on the status of the hearing nerve.
Other causes of conductive hearing loss are: infection; tumors; middle ear fluid from infection or Eustachian tube dysfunction; foreign body; and trauma (as in a skull fracture). Acute infections are usually treated with antibiotic or antifungal medications. Chronic ear infections, chronic middle fluid, and tumors usually require surgery. If there is no response to initial medical therapy, infectious middle ear fluid is usually treated with antibiotics — while chronic non-infectious middle ear fluid is treated with surgery (or pressure equalizing tubes).
Conductive hearing loss from head trauma is frequently amenable to surgical repair of the damaged middle ear structures, performed after the patient’s general medical status is stabilized following acute traumatic injuries.
A genetic form of conductive hearing loss is otosclerosis, in which there is bony fixation of the stapes (the third little bone of hearing in the middle ear), where sound can’t get to the middle ear. Otosclerosis usually presents with hearing loss in early adulthood. Otosclerosis can successfully be managed with surgery to replace the immobile stapes with a mobile stapes prosthesis or with a hearing aid. Research suggests that the measles virus may contribute to stapes fixation in those with a genetic predisposition to otosclerosis. The incidence of otosclerosis may be decreasing in some communities due to measles vaccination. Otosclerosis (a hereditary disorder in which a bony growth forms around a small bone in the middle ear, preventing it from vibrating when stimulated by sound) usually causes a conductive hearing loss, a hearing loss caused by a problem in the outer or middle ear. Less frequently, otosclerosis may cause a sensorineural hearing loss (damaged sensory cells and/or nerve fibers of the inner ear), as well as a conductive hearing loss.
Sensorineural hearing loss (SNHL)
when hearing, loss is due to problems of the inner ear, also known as nerve-related hearing loss.
Causes:
- Exposure to loud noise
- Head trauma
- Virus or disease
- Autoimmune inner ear disease
- Hearing loss that runs in the family
- Aging (Presbycusis)
- Malformation of the inner ear
- Meniere’s Disease
- Otosclerosis – a hereditary disorder in which a bony growth forms around a small bone in the middle ear, preventing it from vibrating when stimulated by sound.
- Tumors
Treatments of Sensorineural Hearing Loss:
- Sensorineural hearing loss can result from acoustic trauma (or exposure to excessively loud noise), which may respond to medical therapy with corticosteroids to reduce cochlea hair cell swelling and inflammation to improve healing of these injured inner ear structures.
- Sensorineural hearing loss can occur from head trauma or abrupt changes in air pressure such as in airplane descent, which can cause inner ear fluid compartment rupture or leakage, which can be toxic to the inner ear. There has been variable success with emergency surgery when this happens.
- Sudden sensorineural hearing loss, presumed to be of viral origin, is an otologic emergency that is medically treated with corticosteroids.
- Bilateral progressive hearing loss over several months, also diagnosed as autoimmune inner ear disease, is managed medically with long-term corticosteroids and sometimes with drug therapy. Autoimmune inner ear disease is when the body’s immune system misdirects its defenses against the inner ear structures to cause damage in this part of the body.
- Fluctuating sensorineural hearing loss may be from unknown cause or associated with Meniere’s Disease. Symptoms of Meniere’s disease are hearing loss, tinnitus (or ringing in the ears), and vertigo. Meniere’s disease may be treated medically with a low-sodium diet, diuretics, and corticosteroids. If the vertigo is not medically controlled, then various surgical procedures are used to eliminate the vertigo.
- Sensorineural hearing loss from tumors of the balance nerve adjacent to the hearing nerve, generally are not reversed with surgical removal or irradiation of these benign tumors. If the hearing loss is mild and the tumors are very small, hearing may be saved in 50 percent of those undergoing hearing preservation surgery for tumor removal.
- Sensorineural hearing loss from disease in the central nervous system may respond to medical management for the specific disease affecting the nervous system. For example, hearing loss secondary to multiple sclerosis may be reversed with treatment for multiple sclerosis.
- Irreversible sensorineural hearing loss, the most common form of hearing loss, may be managed with hearing aids. When hearing aids are not enough, this type of hearing loss can be surgically treated with cochlear implants.
Mixed hearing loss
Refers to a combination of conductive and sensorineural hearing loss. This means that there may be damage in the outer or middle ear and in the inner ear (cochlea) or auditory nerve.
Treatments of Mixed Hearing Loss:
Audiologist recommends taking care of the conductive component first. There have been times when the addition of the conductive component made the person a better hearing aid candidate, by flattening out the audiogram for example, while the underlying sensorineural component presented a high-frequency loss. However, still the emphasis would be on treating medically what can be treated. They say that, generally, you would expect positive results.
Other Causes of Hearing Loss
There are many causes of hearing loss that are beyond our control, such as those caused by heredity. We can’t pick our parents and our genetic make-up – though with continuing advances in gene research, clinical applications, this may be changing. But for now, we have to deal with the hand that heredity has dealt us.
In Some Cases, Hearing Loss Can be Prevented
Ototoxic Drugs
These are medications that are toxic to the ears and can cause hearing loss, sometimes accompanied by tinnitus. We may have some options; however, about the medications we take. It is always a good idea to ask a physician if a hearing loss is one of the possible side-effects. If it is, and there is a substitute medication that would work just as well, then that would be the one to take.
Examples of Otoxic Drugs
- some over-the-counter drugs such as aspirin in high doses
- some antibiotics
- some chemotherapy drugs
- loop diuretics
- some anti-inflammatory drugs
Signs of Ototoxicity (in order of frequency)
- Development of tinnitus in one or both ears
- Intensification of existing tinnitus or the appearance of a new sound
- Fullness or pressure in the ears other than being caused by infection
- Hearing loss in an unaffected ear or the progression o an existing loss.
- Development of vertigo or a spinning sensation usually aggravated by motion which may or may not be accompanied by nausea
Noise-Induced Hearing Loss – Completely Preventable
- A major cause of hearing loss in our society is noise exposure. Tiny hair cells in the ear are damaged when assaulted by loud noise. Once those hair cells are destroyed they cannot be replaced.
- A noise-induced hearing loss is the most common cause for its occurrence in our society and it’s completely preventable.
- Repeated and lengthy exposure to loud sound – whether is it music or a jackhammer – will eventually produce a sensorineural hearing loss.
Damage Risk Criterion
As the sound level increases, the time span one can be exposed to it is reduced. Each day we create more hearing losses in our society with our tolerance of the ear-shattering cacophony that surrounds us.
Musicians
Musicians are particularly at risk. It is their job to listen to the sounds that they and their group are producing, and these may be as high as 135 dB. They have no choice to do this as often as daily; this is their career and their livelihood. Musicians earplugs are available that can help. The newest and best version reduce the sound equally all across the spectrum, from low to high frequencies. Everything sounds just as good as it did before, only softer.
A less expensive, though still effective earplug, can be obtained for the students in a school music program. How to Reduce the Damage to Hearing from Noise
Your ears can be your warning system for potentially dangerous noises. The noise is too loud when:
- You have to raise your voice to be understood by someone standing nearby
- The noise hurts your ears
- You develop a buzzing or ringing sound in your ears, even temporarily (indicates some hair cells have died)
- You don’t hear as well as you normally do until several hours after you get away from the noise.
How to Protect Yourself When Around Loud Noise
- Block the noise (wear earplugs or earmuffs)
- Avoid the noise (put hands over ears if you can’t walk away)
- Turn down the volume
Decibel Loudness Comparison Chart Painful
- 150 dB = fireworks at 3 feet
- 140 dB = firearms, jet engine
- 130 dB = jackhammer
- 120 dB = jet plane takeoff, siren
Extremely Loud
- 110 dB = maximum output of some MP3 players, model airplane, chain saw
- 106 dB = gas lawn mower, snow blower
- 100 dB = hand drill, pneumatic drill
- 90 dB = subway, passing motorcycle
Very Loud
- 80–90 dB = blow-dryer, kitchen blender, food processor
- 70 dB = busy traffic, vacuum cleaner, alarm clock
Moderate
- 60 dB = typical conversation, dishwasher, clothes dryer
- 50 dB = moderate rainfall
- 40 dB = quiet room
- Faint
- 30 dB = whisper, quiet library
*Visit our clinic for more details on Types of Hearing aids and the ones that may be most suitable for you.
What is Tinnitus?
Tinnitus is experiencing noises or ringing in the ears or head when no such external physical noise is present. Tinnitus is usually caused by a fault in the hearing system; it is a symptom, not a disease in itself. The word “tinnitus” means “tinkling or ringing like a bell”. Latin origin; usually pronounced tinn-itus, the “i” as in “sit”. About one in five people with tinnitus have bothersome tinnitus, which distresses them and negatively affects their quality of life and/or functional health status. Those individuals with persistent and bothersome tinnitus will often seek medical care. Tinnitus may be an intermittent or continuous sound in one or both ears. Its pitch can go from a low roar to a high squeal or whine or it can have many sounds. Persistent tinnitus is tinnitus that lasts more than six months. Prior to any treatment, it is important to undergo a thorough examination and evaluation by your otolaryngologist (ENT doctor) and audiologist. An essential part of the treatment will be your understanding of tinnitus and its causes.
What cause Tinnitus?
Many causes – almost everything that can go wrong with our ears can produce tinnitus as a symptom! Perhaps as simple as wax against the eardrum, or as serious as a tumour on the hearing nerve. Otosclerosis (fixation of the tiny stirrup bone in the middle ear) can produce tinnitus; so can Meniere’s disease. A major cause of tinnitus is EXPOSURE TO EXCESSIVE NOISE, e.g. chain saws, machinery, rock concerts. Noise destroys! Most of the time, the tinnitus is subjective—that is, the tinnitus is heard only by the individual. Rarely, tinnitus is “objective,” meaning that the examiner can actually listen and hear the sounds the patient hears. Tinnitus may be caused by different parts of the hearing system. The outer Ear (pinna and ear canal) may be involved. Excessive ear wax, especially if the wax touches the ear drum, causing pressure and changing how the ear drum vibrates, can result in tinnitus. There are a number of non-auditory conditions and lifestyle factors that are associated with tinnitus. Medical conditions such as temporomandibular joint arthralgia (TMJ), depression, anxiety, insomnia, and muscular stress and fatigue may cause tinnitus, or can contribute to worsening of existing tinnitus.
What Can Make Tinnitus Worse?
- Loud Noise
- Stress and Fatigue
- Medications
What testing do i need?
When you are evaluated for tinnitus, the first thing the doctor will do is obtain a complete history, investigating potential causative factors, and perform a thorough, targeted physical examination. If the tinnitus is one-sided (unilateral), associated with hearing loss, or persistent, an audiogram (hearing test) should be obtained early in the evaluation. You may opt for an audiogram in any case. There is no need for radiologic testing (X-rays, CT scans or MRI scans) unless your tinnitus is unilateral, pulsatile, or associated with asymmetric hearing loss or neurological abnormalities. Your doctor will try to determine how bothersome your tinnitus is, by asking certain questions or having you complete a self-assessment questionnaire.
Do Many People Suffer from Tinnitus?
Yes, millions around the world! Probably 18% of Indians have tinnitus at some time of their lives and approximately ’50 million Americans have tinnitus in some form’. Countries with self-help groups include USA, UK, Germany, Canada, New Zealand and, of course, India. Severe tinnitus is recognised as a very major affliction, but most people have tinnitus to a milder degree. Given time, commitment and up-to-date professional help, tinnitus can reduce for many people.
How is Tinnitus treated?
- Hearing Aids
Good quality and properly fitted hearing aids reduce and even eliminate most tinnitus associated with hearing losses. Hearing aids take away the strain of listening and distract from the tinnitus by bringing you more environmental sounds from the outside world.
- Therapeutic Noise Generator
Device which looks like a hearing aid and recommended for people with no hearing loss. It produces a blend of external sounds which stimulate most fibres of the hearing nerve helping to deviate attention away from the tinnitus.
Is there any operation to cure tinnitus?
For the vast majority of people there is no specific operation for tinnitus. However, following successful surgical treatment for some ear problems, an existing tinnitus may sometimes disappear, e.g. otosclerosis, Meniere’s disease, middle ear infection.
Hearing loss in Children
Symptoms in Children
- Very young infants (more than 3-4 months) do not startle at loud noises.
- Does not turn to the source of a sound after 6 months of age.
- Does not say single words, such as “dada” or “mama” by 1 year of age.
- Turns head when he or she sees you but not if you only call out his or her name. This sometimes is mistaken for not paying attention or just ignoring, but could be the result of a partial or complete hearing loss.
- Seems to hear some sounds but not others.
- Outcome of Hearing loss in Children
- Speech is delayed.
- Speech is not clear.
- Does not follow directions. This sometimes is mistaken for not paying attention or just ignoring, but could be the result of a partial or complete hearing loss.
- Turns the TV volume up too high
- Often says, “Huh?”
Who tests hearing in children?
A specialist who tests a person’s hearing is called an audiologist. An audiologist has an advanced degree in diagnostic hearing testing techniques and auditory rehabilitation for children and adults. However, because testing hearing in children requires specific equipment, setup, and training, not all audiologists test children.
Can very young children have their hearing tested?
A child of any age can be tested with the appropriate hearing test. The type of test utilized depends on the child’s age in years or developmental level. Some hearing tests require no behavioural response from the child, while other tests utilize games that entice a child’s interest. The key is to find the right test method for each child.
Causes of Hearing Loss in Children
Hearing loss in children can be broadly classified into: Congenital type & Acquired type
Congenital Causes
The term congenital hearing loss implies that the hearing loss is present at birth. It can include hereditary hearing loss or hearing loss due to other factors present either in utero (prenatal) or at the time of birth.
Genetic factors are thought to cause more than 50% of all incidents of congenital hearing loss in children (4). Genetic hearing loss may be autosomal dominant, autosomal recessive, or X-linked (related to the sex chromosome).
In autosomal dominant hearing loss, one parent who carries the dominant gene for hearing loss and typically has a hearing loss passes it on to the child. In this case there is at least a 50% probability that the child will also have a hearing loss. The probability is higher if both parents have the dominant gene (and typically both have a hearing loss) or if both grandparents on one side of the family have hearing loss due to genetic causes. Because at least one parent usually has a hearing loss, there is prior expectation that the child may have a hearing loss.
In autosomal recessive hearing loss , both parents who typically have normal hearing, carry a recessive gene. In this case the probability of the child having a hearing loss is 25%. Because both parents usually have normal hearing, and because no other family members have hearing loss, there is no prior expectation that the child may have a hearing loss.
In X-linked hearing loss, the mother carries the recessive trait for hearing loss on the sex chromosome and passes it on to males, but not to females.
There are some genetic syndromes,in which, hearing loss is one of the known characteristics. Some examples are Down syndrome (abnormality on a gene), Usher syndrome (autosomal recessive), Treacher Collins syndrome (autosomal dominant), Crouzon syndrome (autosomal dominant), and Alport syndrome (X-linked).
Other causes of congenital hearing loss that are not hereditary in nature include prenatal infections, illnesses, toxins consumed by the mother during pregnancy or other conditions occurring at the time of birth or shortly thereafter. These conditions typically cause Sensori- neural hearing loss ranging from mild to profound in degree. Examples include:
- Intrauterine infections including rubella (German measles), cytomegalovirus, and herpes simplex virus
- Complications associated with the Rh factor in the blood
- Prematurity
- Maternal diabetes
- Toxemia during pregnancy
- Lack of oxygen (anoxia)
Acquired Causes
Acquired hearing loss is a hearing loss, which appears after birth, at any time in one’s life, perhaps as a result of a disease, a condition, or an injury. The following are examples of conditions that can cause acquired hearing loss in children are:
- Ear infections (otitis media) (link to specific section)
- Ototoxic (damaging to the auditory system) drugs
- Meningitis
- Measles
- Encephalitis
- Chicken pox
- Influenza
- Mumps
- Head injury
- Noise exposure
- Ear wax
Treatments
Early hearing loss can affect how a child learns language, which experts believe starts during the first months of life. If problems get diagnosed and treated quickly, babies and children can avoid trouble with language.
The right treatment for a child who can’t hear depends on what caused the problem and how much he can’t hear.
The most common treatments for otitis media include:
Watchful waiting. The condition often goes away on its own, so sometimes the first treatment is simply to watch for changes.
Medications. Your Doctor may prescribe antibiotics or other meds for your child.
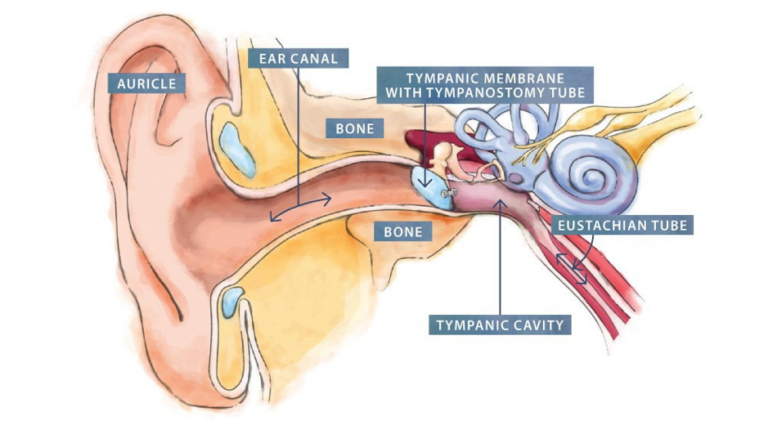
Ear tubes. If the problem doesn’t go away and seems to be affecting your child’s hearing, your Doctor may suggest your child get these tubes. These allow fluid to drain, and they can help prevent infections. If your Doctor thinks your child needs them, she’ll refer you to an ear, nose, and throat (ENT) doctor, also called an otolaryngologist. Your child will need minor surgery to get the ear tubes put in. In a hospital, he’ll get medicine so he’ll be asleep during the operation, but he should be able to go home when it’s over.
Other treatments for children with hearing loss include:
Hearing aids. Children can begin to use these as young as 1 month old. A hearing specialist will help make sure that your child gets the right device.
Implants. Many children and adults get cochlear implants, which are electronic devices that doctors put in the inner ear to help with hearing. They’re usually only for children with serious hearing problems after hearing aids haven’t helped.
Many other devices can help children with hearing loss. Ask a hearing specialist about what might be right for your child. If your child needs ongoing help in school, work with his administrators to see how he can get it. As he grows, it’s likely that his education program will need to adjust. Stay in touch with his teachers and other school professionals to figure out what he needs.
With early treatment and support, children with hearing loss are more likely to learn to communicate and to participate in school and other activities.
Here are a few things you can do to help your child — and yourself:
Get educated. Web sites, as well as government and nonprofit groups, can help you keep up with the latest research.
Communicate. Connect with support groups and online chat communities for parents of children with hearing loss. They know what you’re going through and can give you a lot of information, advice, and understanding.
Stay in touch with your child. Some children with hearing loss feel isolated from other kids their age. But early treatment and hearing aids can reduce the chances they’ll feel alone.
Take care of yourself and your other relationships. Getting help for children can take a lot of time. But don’t forget about your own well-being or other people in your life. Make time for your spouse or partner, stay in touch with friends, and do things you enjoy.
Hearing loss in Children
Symptoms in Children
- Very young infants (more than 3-4 months) do not startle at loud noises.
- Does not turn to the source of a sound after 6 months of age.
- Does not say single words, such as “dada” or “mama” by 1 year of age.
- Turns head when he or she sees you but not if you only call out his or her name. This sometimes is mistaken for not paying attention or just ignoring, but could be the result of a partial or complete hearing loss.
- Seems to hear some sounds but not others.
- Outcome of Hearing loss in Children
- Speech is delayed.
- Speech is not clear.
- Does not follow directions. This sometimes is mistaken for not paying attention or just ignoring, but could be the result of a partial or complete hearing loss.
- Turns the TV volume up too high
- Often says, “Huh?”
Who tests hearing in children?
A specialist who tests a person’s hearing is called an audiologist. An audiologist has an advanced degree in diagnostic hearing testing techniques and auditory rehabilitation for children and adults. However, because testing hearing in children requires specific equipment, setup, and training, not all audiologists test children.
Can very young children have their hearing tested?
A child of any age can be tested with the appropriate hearing test. The type of test utilized depends on the child’s age in years or developmental level. Some hearing tests require no behavioural response from the child, while other tests utilize games that entice a child’s interest. The key is to find the right test method for each child.
Causes of Hearing Loss in Children
Hearing loss in children can be broadly classified into: Congenital type & Acquired type
Congenital Causes
The term congenital hearing loss implies that the hearing loss is present at birth. It can include hereditary hearing loss or hearing loss due to other factors present either in utero (prenatal) or at the time of birth.
Genetic factors are thought to cause more than 50% of all incidents of congenital hearing loss in children (4). Genetic hearing loss may be autosomal dominant, autosomal recessive, or X-linked (related to the sex chromosome).
In autosomal dominant hearing loss, one parent who carries the dominant gene for hearing loss and typically has a hearing loss passes it on to the child. In this case there is at least a 50% probability that the child will also have a hearing loss. The probability is higher if both parents have the dominant gene (and typically both have a hearing loss) or if both grandparents on one side of the family have hearing loss due to genetic causes. Because at least one parent usually has a hearing loss, there is prior expectation that the child may have a hearing loss.
In autosomal recessive hearing loss , both parents who typically have normal hearing, carry a recessive gene. In this case the probability of the child having a hearing loss is 25%. Because both parents usually have normal hearing, and because no other family members have hearing loss, there is no prior expectation that the child may have a hearing loss.
In X-linked hearing loss, the mother carries the recessive trait for hearing loss on the sex chromosome and passes it on to males, but not to females.
There are some genetic syndromes,in which, hearing loss is one of the known characteristics. Some examples are Down syndrome (abnormality on a gene), Usher syndrome (autosomal recessive), Treacher Collins syndrome (autosomal dominant), Crouzon syndrome (autosomal dominant), and Alport syndrome (X-linked).
Other causes of congenital hearing loss that are not hereditary in nature include prenatal infections, illnesses, toxins consumed by the mother during pregnancy or other conditions occurring at the time of birth or shortly thereafter. These conditions typically cause Sensori- neural hearing loss ranging from mild to profound in degree. Examples include:
- Intrauterine infections including rubella (German measles), cytomegalovirus, and herpes simplex virus
- Complications associated with the Rh factor in the blood
- Prematurity
- Maternal diabetes
- Toxemia during pregnancy
- Lack of oxygen (anoxia)
Acquired Causes
Acquired hearing loss is a hearing loss, which appears after birth, at any time in one’s life, perhaps as a result of a disease, a condition, or an injury. The following are examples of conditions that can cause acquired hearing loss in children are:
- Ear infections (otitis media) (link to specific section)
- Ototoxic (damaging to the auditory system) drugs
- Meningitis
- Measles
- Encephalitis
- Chicken pox
- Influenza
- Mumps
- Head injury
- Noise exposure
- Ear wax
Treatments
Early hearing loss can affect how a child learns language, which experts believe starts during the first months of life. If problems get diagnosed and treated quickly, babies and children can avoid trouble with language.
The right treatment for a child who can’t hear depends on what caused the problem and how much he can’t hear.
The most common treatments for otitis media include:
Watchful waiting. The condition often goes away on its own, so sometimes the first treatment is simply to watch for changes.
Medications. Your Doctor may prescribe antibiotics or other meds for your child.
Ear tubes. If the problem doesn’t go away and seems to be affecting your child’s hearing, your Doctor may suggest your child get these tubes. These allow fluid to drain, and they can help prevent infections. If your Doctor thinks your child needs them, she’ll refer you to an ear, nose, and throat (ENT) doctor, also called an otolaryngologist. Your child will need minor surgery to get the ear tubes put in. In a hospital, he’ll get medicine so he’ll be asleep during the operation, but he should be able to go home when it’s over.
Other treatments for children with hearing loss include:
Hearing aids. Children can begin to use these as young as 1 month old. A hearing specialist will help make sure that your child gets the right device.
Implants. Many children and adults get cochlear implants, which are electronic devices that doctors put in the inner ear to help with hearing. They’re usually only for children with serious hearing problems after hearing aids haven’t helped.
Many other devices can help children with hearing loss. Ask a hearing specialist about what might be right for your child. If your child needs ongoing help in school, work with his administrators to see how he can get it. As he grows, it’s likely that his education program will need to adjust. Stay in touch with his teachers and other school professionals to figure out what he needs.
With early treatment and support, children with hearing loss are more likely to learn to communicate and to participate in school and other activities.
Here are a few things you can do to help your child — and yourself:
Get educated. Web sites, as well as government and nonprofit groups, can help you keep up with the latest research.
Communicate. Connect with support groups and online chat communities for parents of children with hearing loss. They know what you’re going through and can give you a lot of information, advice, and understanding.
Stay in touch with your child. Some children with hearing loss feel isolated from other kids their age. But early treatment and hearing aids can reduce the chances they’ll feel alone.
Take care of yourself and your other relationships. Getting help for children can take a lot of time. But don’t forget about your own well-being or other people in your life. Make time for your spouse or partner, stay in touch with friends, and do things you enjoy.
Otitis Media with Effusion (OME)
What is otitis media with effusion (OME)?
Otitis media with effusion (OME) is a collection of non-infected fluid in the middle ear space. It is also called serous or secretory otitis media (SOM). This fluid may accumulate in the middle ear as a result of a cold, sore throat or upper respiratory infection.
OME is usually self-limited, which means, the fluid usually resolves on its own within 4 to 6 weeks. However, in some instances the fluid may persist for a longer period of time and cause a temporary decrease in hearing or the fluid may become infected (acute otitis media).
OME is more common in children between 6 months and 3 years of age, and affects more boys than girls. The condition occurs more often in the fall and winter months and is commonly underdiagnosed because of its lack of acute or obvious symptoms (compared to acute otitis media (AOM).
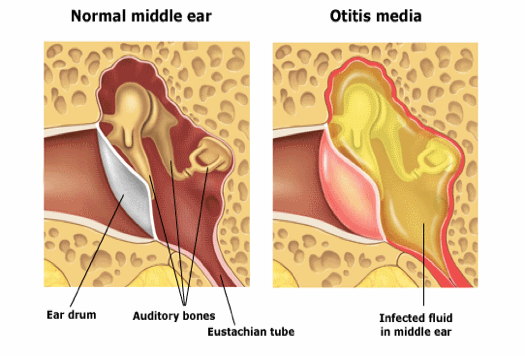
ASOM (Acute Suppurative Otitis Media)
In the United States, acute otitis media (AOM), defined by convention as the first 3 weeks of a process in which the middle ear shows the signs and symptoms of acute inflammation, is the most common affliction necessitating medical therapy for children younger than 5 years. [1, 2, 37] See the image below.

Tympanic membrane of a person with 12 hours of ear pain, slight tympanic membrane bulge, and slight meniscus of purulent effusion at bottom of tympanic membrane.
Signs and symptoms
Although the history of AOM varies with age, a number of constant features manifest during the otitis-prone years, including the following:
Neonates: Irritability or feeding difficulties may be the only indication of a septic focus
Older children: This age group begins to demonstrate a consistent presence of fever and otalgia, or ear tugging
Older children and adults: Hearing loss becomes a constant feature of AOM and otitis media with effusion (OME); ear stuffiness is noted before the detection of middle ear fluid
Ear pain without hearing loss or fever is observed in adults with external otitis media, dental abscess, or pain referred from the temporomandibular joint. Orthodontic appliances often elicit referred pain as the dental occlusion is altered. Diagnosis
Pneumatic otoscopy is the standard of care in the diagnosis of acute and chronic otitis media. The following findings may be found on examination in patients with AOM:
- Signs of inflammation in the tympanic membrane
- Bulging in the posterior quadrants of the tympanic membrane may bulge; scalded appearance of the superficial epithelial layer
- Perforated tympanic membrane (most frequently in posterior or inferior quadrants)
- Presence of an opaque serumlike exudate oozing through the entire tympanic membrane
- Pain with/without pulsation of the otorrhea
- Fever
Testing
Testing in the acute phase is generally unhelpful, because all children with AOM have conductive hearing loss associated with the middle ear effusion. In addition, although tympanometry may assist in the diagnosis of middle ear effusion, this test is seldom necessary for the skilled pneumatic otoscopist.
Culture and sensitivity of a specimen from a fresh perforation or a tympanocentesis may be helpful. Imaging studies
Radiologic studies are generally unnecessary in uncomplicated AOM. However, CT scanning may be necessary to determine if a complication has occurred. MRI might be more appropriate for diagnosing suspected intracranial complications.
Procedure
No surgical procedures are required in majority of the cases of ASOM. However, Tympanocentesis i.e. aspiration of the contents of the middle ear cleft by piercing the tympanic membrane with a needle and collecting that material for diagnostic examination can be offered in some select cases. E.g.
- Neonates who are younger than 6 weeks (and therefore are more likely to have an unusual or more invasive pathogen)
- Immunosuppressed or immunocompromised patients
- Patients in whom adequate antimicrobial treatment has failed and who continue to show signs of local or systemic sepsis
- Patients with a complication that requires a culture for adequate therapy
Management
Pharmacotherapy
Antibiotics are the only medications with demonstrated efficacy in the management of AOM; therefore, these agents are the initial therapy of choice. The antibiotic chosen should cover most of the common bacterial pathogens and be individualized for the child with regard to allergy, tolerance, and previous exposure to antibiotics, cost, and community resistance levels. Duration of treatment may also be a consideration in the choice of antibiotic.
Common antibiotics used in the management of AOM include the following:
- Amoxicillin
- Amoxicillin/clavulanate
- Erythromycin base/sulfisoxazole
- Trimethoprim-sulfamethoxazole
- Cefixime
- Cefuroxime axetil
- Cefprozil
- Cefpodoxime
- Cefdinir
- Clindamycin
- Clarithromycin
- Azithromycin
- Ceftriaxone
Surgery ( rarely required)
Surgical management of AOM can be divided into the following 3 related procedures:
- Tympanocentesis
- Myringotomy
- Myringotomy with insertion of a ventilating tube
Selection of the appropriate procedure results from evaluation of patient factors, surgeon factors, available resources, and urgency.
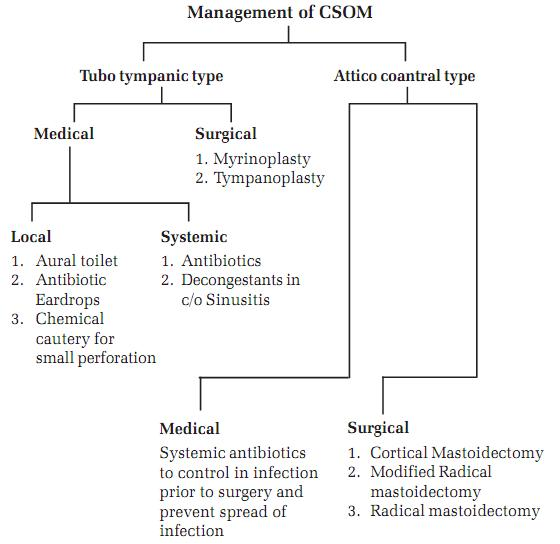
Chronic Suppurative Otitis Media
What is chronic suppurative otitis media?
Chronic suppurative otitis media is chronic infection in part or whole of the middle ear cleft.
What are the different types of chronic suppurative otitis media (CSOM)?
1. Tubotympanic type: (safe type)
Causes:
Usually sequelae of acute otitis media infection, leaving behind a perforation. Recurrent infections via the eustachian tube (tube connecting Middle ear with back of Nose: nasopharynx) commonly from the tonsils or adenoids Traumatic perforation.
Clinical features:
- Perforation: It is usually a central perforation with a safe margin of healthy remanant tympanic membrane around it in the pars tensa.
- Hearing loss: It is a purely conductive type of hearing loss, rarely exceeding 40-45 db.
- Discharge: It is mucoid, copious, non-foul smelling and is related to a bout of upper respiratory tract infection.
- A quiescent phase in the ear symptoms may be present.
2. Atticoantral type: (unsafe type)
It involves the posterio-superior part of the middle ear cleft and is usually associated with cholesteatoma. Aetiology:
- Congenital: These are squamous epithelial cell nests arising within the temporal bone.
- Acquired:
- Primary: Develops in continuity with the pars flacida of the tympanic membrane
- Secondary: This can occur by:
- Immigration of the tympanic membrane epithelium
- Metaplasia: Middle ear mucosa undergoes metaplasia due to repeated infections.
- Negative middle ear pressure.
Clinical features:
- Perforation: It is usually in attic region, postero-superior region, or marginal.
- Retraction pocket: A retraction or invagination of the tympanic membrane is seen in attic or postero-superior region of pars tensa
- Cholesteatoma: This can be seen in the form of pearly white flakes.
What are the investigations required to confirm the diagnosis of chronic suppurative otitis media (CSOM)?
- Suction Microscopy: To suck out any discharge, confirm clinical findings and examination of the discharge for pus culture and antibiotic sensitivity.
- Tuning fork tests: They help in clinical evaluation of hearing loss.
- Pure tone audiogram: This is useful for a qualitative and quantitative analysis of the patients hearing. It also helps for pre-operative and post operative assessment of the hearing loss and for medico-legal purposes.
- X-ray mastoid Schuller’s view: To diagnose the extent of disease and status of the mastoid air cells
- Routine blood investigations from fitness point of view.
- High resolution CT scan of the temporal bone is extremely useful in patients with complications or impending complications.
What is the treatment for chronic suppurative otitis media (CSOM)?
1) Tubotympanic type
A) Medical:
- Local
- Aural toilet
- Antibiotic ear drops
- Chemical cautery for small perforations
- Systemic
- Antibiotics
- Decongestant in case of sinusitis.
- Antioxidants
B) Surgical
- Myringoplasty
- Tympanoplasty with or without a mastoidectomy.
2) Atticoantral Type:
A) Medical:
- Systemic antibiotics to control the infection prior to surgery and prevent spread of infection.
- Medical line of treatment has limited role in unsafe CSOM.
B) Surgical:
- Cortical mastoidectomy
- Modified radical mastoidectomy
- Radical mastoidectomy.
Otitis Externa
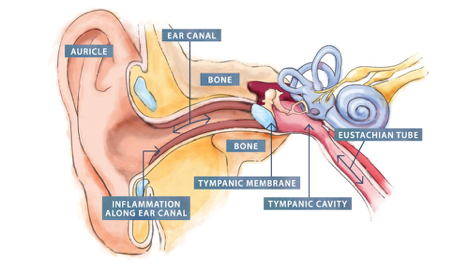
Otitis externa is a condition that causes inflammation (redness and swelling) of the external ear canal, which is the tube between the outer ear and eardrum.
Otitis externa is often referred to as “swimmer’s ear” because repeated exposure to water can make the ear canal more vulnerable to inflammation.
Symptoms of otitis externa include:
- ear pain, which can be severe
- itchiness in the ear canal
- a discharge of liquid or pus from the ear
- some degree of temporary hearing loss
Usually only one ear is affected.
With treatment, these symptoms should clear up within a few days. However, some cases can persist for several months or longer
When to see your Doctor
You should see your Doctor if you may have otitis externa.
Your Doctor will ask about your symptoms and whether you regularly use any items that are inserted into your ears, such as hearing aids or ear plugs. They may also examine inside your ear using an instrument called an otoscope.
If you have recurring episodes of otitis externa that haven’t responded to treatment, your Doctor may take a swab of the inside of your ear. This will be tested to help determine what type of infection you have, if any, so appropriate medication can be prescribed.
What causes otitis externa?
Most cases of otitis externa are caused by a bacterial infection, although the condition can also be caused by:
- irritation
- fungal infections
- allergies
There are a number of things that can make you more likely to develop otitis externa, including:
- damaging the skin inside your ear
- regularly getting water in your ear
Getting water in your ear is particularly significant, because this can cause you to scratch inside your ear, and the moisture also provides an ideal environment for bacteria to grow.
Who is affected?
Otitis externa is relatively common. It’s estimated that around 1 in 10 people will be affected by it at some point in their lives. The condition is slightly more common in women than men and is most often diagnosed in adults aged 45 to 75.
People with certain long-term (chronic) conditions are at greater risk of developing the condition. These include:
- eczema
- asthma
- allergic rhinitis
How otitis externa is treated
Otitis externa sometimes gets better without treatment, but it can take several weeks. Your Doctor can prescribe ear drop medication that usually improves the symptoms within a few days. There are a number of different types of ear drops that may be used to treat otitis externa, but they all tend to be used several times a day for about a week.
Your Doctor may refer you to a specialist for further treatment and advice if symptoms are severe or they fail to respond to treatment. Preventing otitis externa
To help reduce your chances of developing otitis externa, you should avoid inserting cotton wool buds and other things into your ears (including your fingers), as this can damage the sensitive skin in your ear canal.
If you’re a regular swimmer, consider using ear plugs when swimming or wearing a swimming cap to cover your ears and protect them from water.
You should also try to avoid getting water, soap or shampoo into your ears when you have a shower or bath.
Complications
Complications of otitis externa are uncommon, but some can be very serious.
One rare complication of otitis externa is malignant otitis externa, which is where an infection spreads from the ear canal into the surrounding bone. This variety is common in diabetics & patients with low immunity (immuno-compromised).
This requires prompt treatment with antibiotics and sometimes surgery, as it can be fatal if left untreated.
Ear Wax
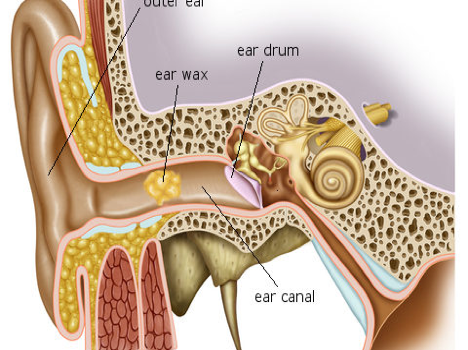
Good intentions to keep ears clean may weaken the ability to hear. The ear is a delicate and intricate body part, including the skin of the ear canal and the eardrum. Therefore, special care should be given to this part of the body. Start by discontinuing the habit of inserting cotton-tipped applicators or other objects into the ear canals.
WHY DOES THE BODY PRODUCE EARWAX?
Cerumen or earwax is healthy in normal amounts and serves as a self-cleaning agent with protective, lubricating, and antibacterial properties. The absence of earwax may result in dry, itchy ears. Self-cleaning means there is a slow and orderly movement of earwax and dead skin cells from the eardrum to the ear opening. Old earwax is constantly being transported, assisted by chewing and jaw motion, from the ear canal to the ear opening where, most of the time, it dries, flakes, and falls out.
Earwax is not formed in the deep part of the ear canal near the eardrum. It is only formed in the outer one-third of the ear canal. So, when a patient has wax blockage against the eardrum, it is often because he has been probing the ear with such things as cotton-tipped applicators, bobby pins, or twisted napkin corners. These objects only push the wax in deeper.
WHEN SHOULD THE EARS BE CLEANED?
Under ideal circumstances, the ear canals should never have to be cleaned. However, that isn’t always the case. The ears should be cleaned when enough earwax accumulates to cause symptoms or to prevent a needed assessment of the ear by your doctor. This condition is call cerumen impaction, and may cause one or more of the following symptoms:
- Earache, fullness in the ear, or a sensation the ear is plugged
- Partial hearing loss, which may be progressive
- Tinnitus, ringing, or noises in the ear
- Itching, odor, or discharge
- Coughing
WHAT IS THE RECOMMENDED METHOD OF EAR CLEANING?
Ideally, ear wax does not need to be cleaned, in fact they offer protection to the skin of outer ear canal from variety of bacterial and fungal infections. They serve similar functions as saliva in mouth or tear in our eyes. However, when the accumulation of ear wax is significant enough to cause hearing loss, Tinnitus or the doctor is unable to have a good view of the ear drums, they can be removed under direct vison by a trained ENT surgeon.
Irrigation or ear syringing is commonly used for cleaning and can be performed by a ENT physician using a commercially available irrigation kit. Common solutions used for syringing include water and saline, which should be warmed to body temperature to prevent dizziness. Ear syringing is most effective when water, saline, or wax dissolving drops are put in the ear canal 15 to 30 minutes before treatment. Caution is advised to avoid having your ears irrigated if you have diabetes, a hole in the eardrum (perforation), tube in the eardrum, skin problems such as eczema in the ear canal or a weakened immune system.
Manual removal of earwax is also effective. This is most often performed by an ENT doctor using suction or special miniature instruments, and a microscope to magnify the ear canal. Manual removal is preferred if your ear canal is narrow, the eardrum has a perforation or tube, other methods have failed, or if you have skin problems affecting the ear canal, diabetes or a weakened immune system.
WHY SHOULDN’T COTTON SWABS BE USED TO CLEAN EARWAX?
Wax blockage is one of the most common causes of hearing loss. This is often caused by attempts to clean the ear with cotton swabs. Most cleaning attempts merely push the wax deeper into the ear canal, causing a blockage.
The outer Ear is the funnel-like part of the ear that can be seen on the side of the head, plus the ear canal (the hole which leads down to the eardrum). The ear canal is shaped somewhat like an hourglass narrowing part way down. The skin of the outer part of the canal has special glands that produce earwax. This wax is supposed to trap dust and dirt particles to keep them from reaching the eardrum. Usually the wax accumulates a bit, dries out, and then comes out of the ear, carrying dirt and dust with it. Or it may slowly migrate to the outside where it can be wiped off.
ARE EAR CANDLES AN OPTION FOR REMOVING WAX BUILD UP?
No, ear candles are not a safe option of wax removal as they may result in serious injury. Since users are instructed to insert the 10- to 15-inch-long, cone-shaped, hollow candles, typically made of wax-impregnated cloth, into the ear canal and light the exposed end, some of the most common injuries are burns, obstruction of the ear canal with wax of the candle, or perforation of the membrane that separates the ear canal and the middle ear.
The U.S. Food and Drug Administration (FDA) became concerned about the safety issues with ear candles after receiving reports of patient injury caused by the ear candling procedure. There are no controlled studies or other scientific evidence that support the safety and effectiveness of these devices for any of the purported claims or intended uses as contained in the labelling.
WHEN SHOULD A DOCTOR BE CONSULTED?
If the home treatments discussed in this leaflet are not satisfactory or if wax has accumulated so much that it blocks the ear canal (and hearing), a physician may prescribe eardrops designed to soften wax, or she may wash or vacuum it out. Occasionally, an otolaryngologist (ear, nose, and throat specialist) may need to remove the wax under microscopic visualization. If there is a possibility of a perforation in the eardrum, consult a physician prior to trying any over-the-counter remedies. Putting eardrops or other products in the ear with the presence of an eardrum perforation may cause pain or an infection. Certainly, washing water through such a hole could start an infection.
WHAT CAN I DO TO PREVENT EXCESSIVE EARWAX?
There are no proven ways to prevent cerumen impaction, but not inserting cotton-tipped swabs or other objects in the ear canal is strongly advised. If you are prone to repeated wax impaction or use hearing aids, consider seeing your doctor every 6 to 12 months for a checkup and routine preventive cleaning.
What You Need to Know
Otomycosis is a fungal infection that affects the ears. It mostly affects people who live in warm or tropical areas. It also often affects people who swim frequently, live with diabetes, or have other chronic medical and skin conditions. There are several treatment options for otomycosis, but it can become chronic.
SYMPTOMS
Symptoms of otomycosis
The following symptoms are common for otomycosis:
- pain
- itching
- inflammation
- swelling
- redness
- flaky skin
- ringing in the ears
- feeling of fullness in the ears
- discharge of fluid from the ears
- hearing problems
Discharge from the ears is one of the most common symptoms and may be different colors. You may see white, yellow, black, gray, or green fluid.
CAUSES
Causes of this condition
A fungus causes otomycosis. There are nearly 60 different species of fungi that may be responsible for this infection. Common fungi include Aspergillus and Candida. Sometimes bacteria can combine with the fungi and make the infection more complicated. Otomycosis is more common in tropical and warm regions because fungi can grow better in these areas. This infection is also more common during the summer months. Fungi need moisture and warmth to grow. People who swim in contaminated water are more likely to get otomycosis. Even swimming or surfing in clean water can increase the risk. In addition, people who have weakened immune systems, trauma or injuries in the ear, eczema, or other chronic skin problems are at a higher risk of getting this type of infection.
DIAGNOSIS
Diagnosing otomycosis
You should see a doctor if there is pain and discharge in your ears. You may need medication to treat the symptoms and discomfort, so a correct diagnosis of otomycosis is necessary.
The doctor will collect your medical history and do a physical exam to diagnose otomycosis. They may use an otoscope, which is a lighted device used to look inside the ears at the eardrum and ear canal. They may swab your ears to run laboratory tests on the discharge, buildup, or fluid. The tests usually include looking at the organisms under a microscope.
TREATMENT
Treatment of otomycosis
There are several treatment options for otomycosis. Talk to your doctor to determine the best one for your fungal infection. Cleaning
Your doctor can thoroughly clean your ears to remove buildup and discharge. They may use rinses or other methods to clean your ears. Don’t try this at home with cotton swabs or use other instruments inside your ears. Cotton swabs should only be used on the outside of the ear.
Ear drops
You may need to use antifungal ear drops to treat otomycosis. They may include clotrimazole and fluconazole. Acetic acid is another common treatment for otomycosis. Usually, a 2 percent solution of these ear drops is used several times a day for about a week. Another option is to use 5 percent aluminum acetate ear drops. Learn how to use ear drops effectively. Oral medications
Some fungal infections such as Aspergillus may be resistant to the usual ear drops. They may require oral medications like itraconazole (Sporanox).
You may also need to take over-the-counter medications such as nonsteroidal anti-inflammatory drugs or acetaminophen (Tylenol) for the pain.
Topical medications
Your doctor may recommend topical antifungal medications for otomycosis. These typically come as ointments or creams. Home remedies
Several home remedies may help treat otomycosis, but you should talk to a doctor before trying them. Diluted hydrogen peroxide may help remove buildup from your ears. Over-the-counter medications that contain carbamide peroxide can also help clear your ears of wax. After swimming, another option is to use an ear-drop solution of equal parts white vinegar and rubbing alcohol.
Wearing a swim cap or earplugs can also keep water out of your ears. You may want to use dry heat such as a hair dryer to remove moisture from the ears. Make sure to use the lowest setting and avoid putting the hair dryer too close to your ears.
Outlook for this condition
In most cases, antifungal treatments are enough to get rid of otomycosis. However, some people don’t respond to these treatments, and otomycosis may become chronic.
If you have diabetes, a weakened immune system, or chronic health problems, getting those conditions under good control is important. Treating any chronic skin conditions, like eczema, is also important.
In addition, continued exposure to the fungus from contaminated water or other sources can cause the infection to return.
PREVENTION
Preventing otomycosis
There are things you can do to help prevent otomycosis:
Prevention tips
- Avoid getting water in your ears while swimming or surfing.
- Dry your ears after showering.
- Avoid putting cotton swabs inside your ears.
- Avoid scratching the skin outside and inside your ears.
- Use acetic acid ear drops after getting water in your ears.
What is otosclerosis?
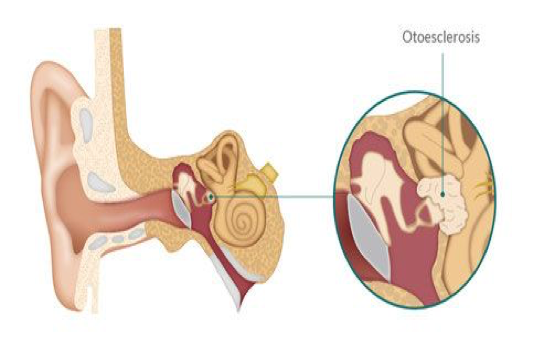
Otosclerosis is a hereditary condition that causes the abnormal growth of bone of the middle ear and inner ear. This bone prevents structures within the ear from working properly and causes hearing loss. For some people with otosclerosis, the hearing loss may become severe.
How does Otosclerosis cause hearing impairment?
Otosclerosis can cause different types of hearing loss, depending on which structure within the ear is affected. Otosclerosis usually affects the last bone in the chain, the stapes, which rests in the entrance to the inner ear (the oval window). The abnormal bone fixates the stapes in the oval window and interferes with sound passing waves to the inner ear. This causes a conductive or mechanical hearing loss, a hearing loss caused by a problem in the outer or middle ear. Less frequently, otosclerosis may cause a sensorineural hearing loss (damaged sensory cells and/or nerve fibers of the inner ear). Most patients with Otosclerosis have a combination of these problems, or a mixed hearing loss. Next commonly, patients may have a pure conductive hearing loss. The least common pattern is a sensorineural pattern which can sometimes be difficult to diagnose as it can mimic hearing loss from other causes. Otolsclerosis may cause mild to profound hearing loss and is very variable amongst those affected.
What causes Otosclerosis?
The cause of otosclerosis is not fully understood, although it is a hereditary problem, or passed down from parent to child. Many different genes seem to be involved in this problem. It can skip generations and be silent and appear to cause hearing loss in a person without a known family history of it. It can cause different severities of hearing loss amongst those affected in the family. It may be completely silent in one person, but be passed on through genetics to their children.
People who have a family history of otosclerosis are more likely to develop the disorder. On average, a person who has one parent with otosclerosis has a 25 percent chance of developing the disorder. If both parents have otosclerosis, the risk goes up to 50 percent. Research shows that white, middle-aged women are most at risk.
Some research suggests a relationship between otosclerosis and the hormonal changes associated with pregnancy. While the exact cause remains unknown, there is some evidence associating viral infections (such as measles) and otosclerosis.
What are the symptoms of otosclerosis?
Hearing loss is the most frequent symptom of otosclerosis. The loss may appear very gradually. Many people with otosclerosis first notice that they cannot hear low-pitched sounds or that they can no longer hear a whisper. In addition to hearing loss, some people with otosclerosis may experience dizziness, balance problems, or tinnitus. Tinnitus is a sensation of ringing, roaring, buzzing, or hissing in the ears or head that accompanies many forms of hearing loss.
How is otosclerosis diagnosed?
Otosclerosis is diagnosed by a careful physical examination and audiolocal testing. The acoustic reflex tests in the immitence part of the hearing evaluation are particularly important to it’s diagnosis. Sometimes the diagnosis takes a few years to establish, with serial audiograms being required when the hearing loss is mild, or the sensorinerual kind of hearing loss is present. A CT scan is occasionally used to confirm its presence.
How is otosclerosis treated?
Medical therapy is sometimes recommended. Fluoride therapy is thought to potentially prevent the development of sensorinerual hearing loss, but will not improve hearing loss that has already developed. Hearing aids are commonly prescribed for patients with otosclerosis. A hearing aid is designed to compensate for a hearing loss by amplifying sound. An audiologist can discuss the various types of hearing aids available and make a recommendation based on the specific needs of an individual.
Surgery is an option for treatment of the conductive or mechanical hearing loss caused by otosclerosis. In an operation called a stapedectomy, or stapedotomy, an otologist (ear surgeon) bypasses the diseased bone with a prosthetic device that allows sound waves to be passed to the inner ear. It is important to discuss the risks and possible complications of this procedure, as well as the benefits, with the surgeon. In rare cases, surgery can worsen the hearing loss.
Stapedectomy/Stapedotomy
A stapes operation can be performed to improve hearing in patients who have a “frozen” or “stuck” stapes bone. This usually occurs in patients who have the condition called otosclerosis, but can occur in other hereditary conditions or in patients who have had very severe middle ear infections or previous surgeries. The stapes is the last hearing bone in the chain of bones in the middle ear, and it is normally mobile and attached by a ligament to an opening of the bone that houses the inner ear, called the oval window. A frozen stapes bone causes a mechanical or conductive hearing loss.
The operation to allow sound to pass into the inner ear again is called a stapedectomy, or stapedotomy, depending on the size of hole made into the oval window, but the operations are pretty much the same. The surgery is usually performed on an out-patient basis and takes about an hour. It is usually performed with sedation, although some patients require general anesthesia. In most cases, the operation can be completed by working through the ear canal, although sometimes an incision needs to be made behind the ear if the ear canal is small or the anatomy is different. A microscope and laser are used.
The ear is completely numbed and incisions are made in the ear canal and the drum is lifted up out of the way. The diagnosis is confirmed by making sure that the other bones are normal. A vein graft from the hand or arm or a tissue graft from behind the ear is obtained through a tiny incision. The top of the stapes bone is removed and an opening is made into the base, or footplate of the stapes bone. A prosthesis made of titanium is placed between the hole and the incus bone and a tissue graft is used to help seal the hole. The drum is put down into position, the hearing is tested and packing is placed in the ear canal.
Post-op Care
After surgery, the patient stays in bed in the hospital for a few hours to prevent nausea and vomiting. The nurses then help the patient get up and walk and if there is no significant dizziness or nausea, the patient can be discharged home.
The patient’s activity is fairly restricted for the first week, and then a gradual return to activity can occur, but heavy exercise, staining, blowing the nose, or lifting anything more than 10 pounds needs to be avoided for 4-6 weeks. The packing is removed in the office one week after surgery and the hearing gradually returns over the next month. Water needs to be kept out of the ear for 2-3 weeks.
Complications
- Nausea and dizziness: this is common and expected after surgery and is usually mild and short lived. Many medications are given to prevent these and only a few patients feel dizzy beyond the day of surgery. Some patients feel sensitive to motion for a few days. Driving is restricted until this resolves, usually no more than a few days. If severe dizziness occurs, the patient is kept in hospital and given medication until it resolves
- Temporary change in taste: A nerve of taste runs under the ear drum and has to be moved out of the way during surgery. This can leave a loss of taste, or taste change on the side of the tongue which is usually temporary.
- No improvement in the hearing, or lack of significant improvement can occur in 2% of cases.
- High frequency hearing loss can occur in 5-10% but the improvement in other frequencies usually makes up for this.
- Tinnitus usually improves with hearing improvement after surgery, but in rare cases can occur or worsen.
- A perforated eardrum or damage to the other ear bones are rare.
- Facial nerve paralysis is extremely rare.
- Total loss of hearing can occur in 1% of cases. If this occurs, a conventional hearing aid would not help restore the hearing loss.
- Some patients develop a recurrence of hearing loss and need to undergo repeat surgery in the future. This probably happens in 5% of patients over their lifetime.
Giddiness due to Benign paroxysmal positional vertigo (BPPV)
Benign paroxysmal positional vertigo (BPPV) is one of the most common causes of vertigo — the sudden sensation that you’re spinning or that the inside of your head is spinning.
Benign paroxysmal positional vertigo causes brief episodes of mild to intense dizziness. Benign paroxysmal positional vertigo is usually triggered by specific changes in the position of your head. This might occur when you tip your head up or down, when you lie down, or when you turn over or sit up in bed.
Although benign paroxysmal positional vertigo can be a bothersome problem, it’s rarely serious except when it increases the chance of falls. You can receive effective treatment for benign paroxysmal positional vertigo during a doctor’s office visit.
Symptoms
The signs and symptoms of benign paroxysmal positional vertigo (BPPV) may include:
- Dizziness
- A sense that you or your surroundings are spinning or moving (vertigo)
- A loss of balance or unsteadiness
- Nausea
- Vomiting
The signs and symptoms of BPPV can come and go, with symptoms commonly lasting less than one minute. Episodes of benign paroxysmal positional vertigo can disappear for some time and then recur.
Activities that bring about the signs and symptoms of BPPV can vary from person to person, but are almost always brought on by a change in the position of your head. Some people also feel out of balance when standing or walking.
Abnormal rhythmic eye movements (nystagmus) usually accompany the symptoms of benign paroxysmal positional vertigo.
When to see a doctor
Generally, see your doctor if you experience any unexplained dizziness or vertigo that recurs periodically for more than one week.
Seek emergency care
Although it’s uncommon for dizziness to signal a serious illness, see your doctor immediately if you experience dizziness or vertigo along with any of the following:
- A new, different or severe headache
- A fever
- Double vision or loss of vision
- Hearing loss
- Trouble speaking
- Leg or arm weakness
- Loss of consciousness
- Falling or difficulty walking
- Numbness or tingling
The signs and symptoms listed above may signal a more serious problem.
Causes
- Often, there’s no known cause for BPPV. This is called idiopathic BPPV.
When a cause can be determined, BPPV is often associated with a minor to severe blow to your head. Less common causes of BPPV include disorders that damage your inner ear or, rarely, damage that occurs during ear surgery or during prolonged positioning on your back, such as in a dentist chair. BPPV also has been associated with migraines.
The ear’s role
Inside your ear is a tiny organ called the vestibular labyrinth. It includes three loop-shaped structures (semicircular canals) that contain fluid and fine, hair-like sensors that monitor the rotation of your head.
Other structures (otolith organs) in your ear monitor movements of your head — up and down, right and left, back and forth — and your head’s position related to gravity. These otolith organs contain crystals that make you sensitive to gravity.
For a variety of reasons, these crystals can become dislodged. When they become dislodged, they can move into one of the semicircular canals — especially while you’re lying down. This causes the semicircular canal to become sensitive to head position changes it would normally not respond to, which is what makes you feel dizzy.
Risk factors
Benign paroxysmal positional vertigo occurs most often in people age 50 and older, but can occur at any age. Benign paroxysmal positional vertigo is also more common in women than in men. A head injury or any other disorder of the balance organs of your ear may make you more susceptible to BPPV.
Complications
Although benign paroxysmal positional vertigo (BPPV) is uncomfortable, it rarely causes complications. The dizziness of BPPV can make you unsteady, which may put you at greater risk of falling.
Diagnosis
Your doctor may do a series of tests to determine the cause of your dizziness. During a physical examination, your doctor will likely look for:
- Signs and symptoms of dizziness that are prompted by eye or head movements and then decrease in less than one minute
- Dizziness with specific eye movements that occur when you lie on your back with your head turned to one side and tipped slightly over the edge of the examination bed
- Involuntary movements of your eyes from side to side (nystagmus)
- Inability to control your eye movements
If the cause of your signs and symptoms is difficult to determine, your doctor may order additional testing, such as:
- Electronystagmography (ENG) or videonystagmography (VNG). The purpose of these tests is to detect abnormal eye movement. ENG (which uses electrodes) or VNG (which uses small cameras) can help determine if dizziness is due to inner ear disease by measuring involuntary eye movements while your head is placed in different positions or your balance organs are stimulated with water or air.
- Magnetic resonance imaging (MRI). This test uses a magnetic field and radio waves to create cross-sectional images of your head and body. Your doctor can use these images to identify and diagnose a range of conditions. MRI may be performed to rule out other possible causes of vertigo.
Treatment
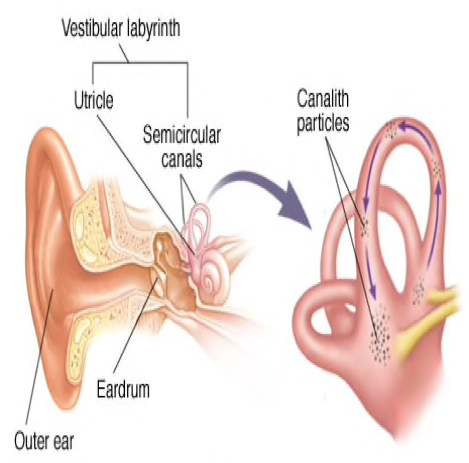
- The inner ear and canalith repositioning
Benign paroxysmal positional vertigo may go away on its own within a few weeks or months. But, to help relieve BPPV sooner, your doctor, audiologist or physical therapist may treat you with a series of movements known as the canalith repositioning procedure.
Canalith repositioning
Performed in your doctor’s office, the canalith repositioning procedure consists of several simple and slow maneuvers for positioning your head. The goal is to move particles from the fluid-filled semicircular canals of your inner ear into a tiny bag-like open area (vestibule) that houses one of the otolith organs in your ear where these particles don’t cause trouble and are more easily resorbed.
Each position is held for about 30 seconds after any symptoms or abnormal eye movements stop. This procedure is usually effective after one or two treatments.
Your doctor will likely teach you how to perform the canalith repositioning procedure on yourself so that you can do it at home if necessary.
Surgical alternative
In very rare situations in which the canalith repositioning procedure isn’t effective, your doctor may recommend a surgical procedure in which a bone plug is used to block the portion of your inner ear that’s causing dizziness. The plug prevents the semicircular canal in your ear from being able to respond to particle movements or head movements in general. The success rate for canal plugging surgery is approximately 90 percent.
Lifestyle and home remedies
If you experience dizziness associated with benign paroxysmal positional vertigo (BPPV), consider these tips:
- Be aware of the possibility of losing your balance, which can lead to falling and serious injury.
- Sit down immediately when you feel dizzy.
- Use good lighting if you get up at night.
- Walk with a cane for stability if you’re at risk of falling.
- Work closely with your doctor to manage your symptoms effectively.
BPPV may recur even after successful therapy. Fortunately, although there’s no cure, the condition can be managed with physical therapy and home treatments.
Preparing for your appointment
Make an appointment with your doctor if you have symptoms common to BPPV. After an initial examination, your doctor may refer you to an ear, nose and throat (ENT) specialist or a doctor who specializes in the brain and nervous system (neurologist). Here’s some information to help you get ready for your appointment.
What you can do
- Write down your symptoms, including when they started and how often they occur.
- Note any recent blows to your head, including even minor accidents or injuries.
- Make a list of your key medical information, including any other conditions for which you’re being treated and the names of any medications, vitamins and supplements you’re taking.
- Write down questions to ask your doctor. Creating your list of questions can help you make the most of your time with your doctor.
