
- GERD (Gastro- Esophageal- Reflux Disease)
- (OSA)Obstructive sleep apnoea
- Acute Tonsillitis
- Oral Sub-mucous Fibrosis
- Thyroid Diseases
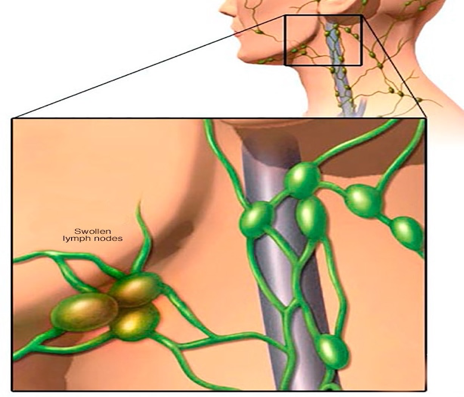
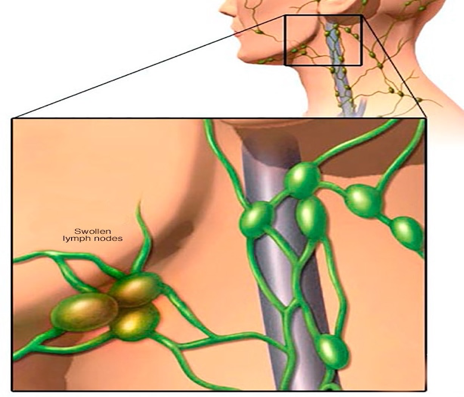
- Swollen Lymph Nodes in Neck
- Stridor (Noisy breathing in newborn or young children)
- Hoarseness or Rough Voice
Overview
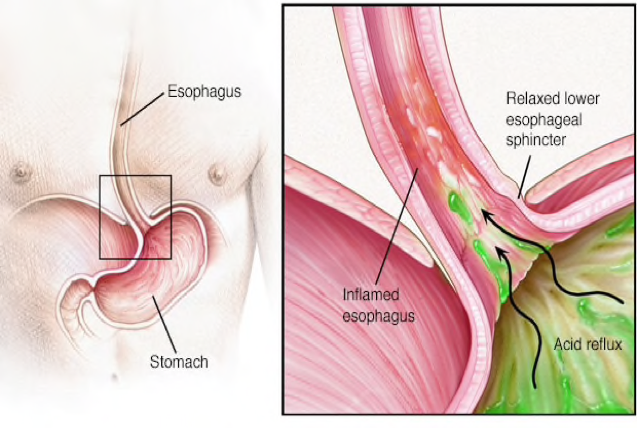
How heartburn and GERD occur
Gastroesophageal reflux disease (GERD) occurs when stomach acid frequently flows back into the tube connecting your mouth and stomach (esophagus). This backwash (acid reflux) can irritate the lining of your esophagus.
Many people experience acid reflux from time to time. GERD is mild acid reflux that occurs at least twice a week, or moderate to severe acid reflux that occurs at least once a week.
Most people can manage the discomfort of GERD with lifestyle changes and over-the-counter medications. But some people with GERD may need stronger medications or surgery to ease symptoms.
Symptoms
Common signs and symptoms of GERD include:
- A burning sensation in your chest (heartburn), usually after eating, which might be worse at night
- Chest pain
- Difficulty swallowing
- Regurgitation of food or sour liquid
- Sensation of a lump in your throat
If you have night-time acid reflux, you might also experience:
- Chronic cough
- Laryngitis
- New or worsening asthma
- Disrupted sleep
When to see a doctor
Seek immediate medical care if you have chest pain, especially if you also have shortness of breath, or jaw or arm pain. These may be signs and symptoms of a heart attack.
Make an appointment with your doctor if you:
- Experience severe or frequent GERD symptoms
- Take over-the-counter medications for heartburn more than twice a week
Causes
GERD is caused by frequent acid reflux.
When you swallow, a circular band of muscle around the bottom of your esophagus (lower esophageal sphincter) relaxes to allow food and liquid to flow into your stomach. Then the sphincter closes again.
If the sphincter relaxes abnormally or weakens, stomach acid can flow back up into your esophagus. This constant backwash of acid irritates the lining of your esophagus, often causing it to become inflamed.
Risk factors
Conditions that can increase your risk of GERD include:
- Obesity
- Bulging of the top of the stomach up into the diaphragm (hiatal hernia)
- Pregnancy
- Connective tissue disorders, such as scleroderma
- Delayed stomach emptying Factors that can aggravate acid reflux include:
- Smoking
- Eating large meals or eating late at night
- Eating certain foods (triggers) such as fatty or fried foods
- Drinking certain beverages, such as alcohol or coffee
- Taking certain medications, such as aspirin
Complications
Over time, chronic inflammation in your esophagus can cause:
- Narrowing of the esophagus (esophageal stricture). Damage to the lower esophagus from stomach acid causes scar tissue to form. The scar tissue narrows the food pathway, leading to problems with swallowing.
- An open sore in the esophagus (esophageal ulcer). Stomach acid can wear away tissue in the esophagus, causing an open sore to form. An esophageal ulcer can bleed, cause pain and make swallowing difficult.
- Precancerous changes to the esophagus (Barrett’s esophagus). Damage from acid can cause changes in the tissue lining the lower esophagus. These changes are associated with an increased risk of esophageal cancer.
(OSA)Obstructive sleep apnoea
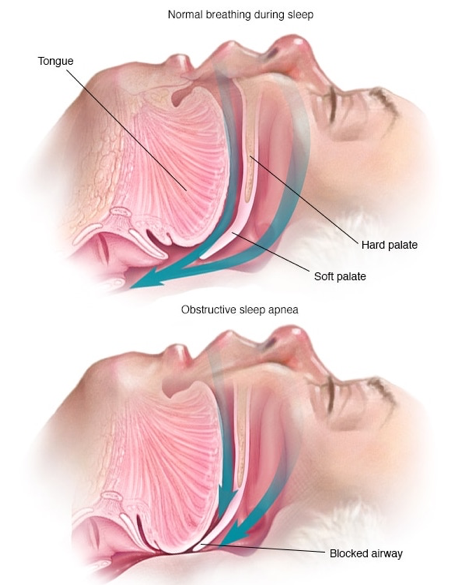
Obstructive sleep apnoea is a potentially serious sleep disorder. It causes breathing to repeatedly stop and start during sleep. There are several types of sleep apnoea, but the most common is obstructive sleep apnoea. This type of apnoea occurs when your throat muscles intermittently relax and block your airway during sleep. A noticeable sign of obstructive sleep apnoea is snoring.
OTreatments for obstructive sleep apnoea are available. One treatment involves using a device that keep your airway open while you sleep. Another option is a mouthpiece to thrust your jaw forward during sleep. In more severe cases, surgery may be an option too.
Symptoms
Signs and symptoms of obstructive sleep apnoea include:
- Excessive daytime sleepiness
- Loud snoring
- Observed episodes of breathing cessation during sleep
- Abrupt awakenings accompanied by gasping or choking
- Awakening with a dry mouth or sore throat
- Morning headache
- Difficulty concentrating during the day
- Experiencing mood changes, such as depression or irritability
- High blood pressure
- Night time sweating
- Decreased libido
When to see a doctor
Consult a medical professional if you experience, or if your partner observes, the following:
- Snoring loud enough to disturb your sleep or that of others
- Waking up gasping or choking
- Intermittent pauses in your breathing during sleep
- Excessive daytime drowsiness, which may cause you to fall asleep while you’re working, watching television or even driving a vehicle
Many people may not think of snoring as a sign of something potentially serious, and not everyone who snores has obstructive sleep apnoea.
Be sure to talk to your doctor if you experience loud snoring, especially snoring that’s punctuated by periods of silence. With obstructive sleep apnoea, snoring usually is loudest when you sleep on your back, and it quiets when you turn on your side. Ask your doctor about any sleep problem that leaves you chronically fatigued, sleepy and irritable. Excessive daytime drowsiness may be due to other disorders, such as narcolepsy.
Causes
Obstructive sleep apnoea occurs when the muscles in the back of your throat relax too much to allow normal breathing. These muscles support structures including the soft palate, the uvula — a triangular piece of tissue hanging from the soft palate, the tonsils and the tongue.
When the muscles relax, your airway narrows or closes as you breathe in and breathing may be inadequate for 10 to 20 seconds. This may lower the level of oxygen in your blood and cause a build up of carbon dioxide. Your brain senses this impaired breathing and briefly rouses you from sleep so that you can reopen your airway. This awakening is usually so brief that you don’t remember it.
You can awaken with a transient shortness of breath that corrects itself quickly, within one or two deep breaths. You may make a snorting, choking or gasping sound.
This pattern can repeat itself five to 30 times or more each hour, all night long. These disruptions impair your ability to reach the desired deep, restful phases of sleep, and you’ll probably feel sleepy during your waking hours. People with obstructive sleep apnoea may not be aware that their sleep was interrupted. In fact, many people with this type of sleep apnoea think they slept well all night.
Risk factors
Anyone can develop obstructive sleep apnoea. However, certain factors put you at increased risk, including:
- Excess weight. Around half the people with obstructive sleep apnoea are overweight. Fat deposits around the upper airway may obstruct breathing.However, not everyone with obstructive sleep apnoea is overweight and vice versa. Thin people can develop the disorder, too.
- Narrowed airway. You may inherit naturally narrow airways. Or, your tonsils or adenoids may become enlarged, which can block your airway.
- High blood pressure (hypertension). Obstructive sleep apnoea is relatively common in people with hypertension.
- Chronic nasal congestion. Obstructive sleep apnoea occurs twice as often in those who have consistent nasal congestion at night, regardless of the cause. This may be due to narrowed airways.
- Smoking. People who smoke are more likely to have obstructive sleep apnoea.
- Diabetes. Obstructive sleep apnoea may be more common in people with diabetes.
- Sex. In general, men are twice as likely as women to have obstructive sleep apnoea.
- A family history of sleep apnoea. If you have family members with obstructive sleep apnoea, you may be at increased risk.
- Asthma. Recent research has found an association between asthma and the risk of obstructive sleep apnoea.
Complications
Obstructive sleep apnoea is considered a serious medical condition. Complications may include:
- Daytime fatigue and sleepiness. The repeated awakenings associated with obstructive sleep apnoea make normal, restorative sleep impossible. People with obstructive sleep apnoea often experience severe daytime drowsiness, fatigue and irritability. They may have difficulty concentrating and find themselves falling asleep at work, while watching TV or even when driving.Children and young people with obstructive sleep apnoea may do poorly in school and commonly have attention or behaviour problems.
- Cardiovascular problems. Sudden drops in blood oxygen levels that occur during obstructive sleep apnoea increase blood pressure and strain the cardiovascular system. Many people with obstructive sleep apnoea develop high blood pressure (hypertension), which can increase the risk of heart disease.The more severe the obstructive sleep apnoea, the greater the risk of coronary artery disease, heart attack, heart failure and stroke. Men with obstructive sleep apnoea appear to be at risk of heart failure, while women with obstructive sleep apnoea don’t.Obstructive sleep apnea increases the risk of abnormal heart rhythms (arrhythmias). These abnormal rhythms can lower blood oxygen levels. If there’s underlying heart disease, these repeated multiple episodes of low blood oxygen could lead to sudden death from a cardiac event.
- Complications with medications and surgery. Obstructive sleep apnoea also is a concern with certain medications and general anaesthesia. These medications, such as sedatives, narcotic analgesics and general anaesthetics, relax your upper airway and may worsen your obstructive sleep apnoea.If you have obstructive sleep apnoea, you may experience worse breathing problems after major surgery, especially after being sedated and lying on your back. People with obstructive sleep apnoea may be more prone to complications after surgery.Before you have surgery, tell your doctor if you have obstructive sleep apnoea or symptoms related to obstructive sleep apnoea. If you have obstructive sleep apnoea symptoms, your doctor may test you for obstructive sleep apnoea prior to surgery.
- Eye problems. Some research has found a connection between obstructive sleep apnoea and certain eye conditions, such as glaucoma. Eye complications can usually be treated.
- Sleep-deprived partners. Loud snoring can keep those around you from getting good rest and eventually disrupt your relationships. Some partners may even choose to sleep in another room. Many bed partners of people who snore are sleep deprived as well. People with obstructive sleep apnoea may also complain of memory problems, morning headaches, mood swings or feelings of depression, and a need to urinate frequently at night (nocturia).
Diagnosis
To diagnose your condition, your doctor may make an evaluation based on your signs and symptoms, an examination, and tests. Your doctor may refer you to a sleep specialist in a sleep centre for further evaluation.
You’ll have a physical examination, and your doctor will examine the back of your throat, mouth and nose for extra tissue or abnormalities. Your doctor may measure your neck and waist circumference and check your blood pressure.
A sleep specialist may conduct additional evaluations to diagnose your condition, determine the severity of your condition and plan your treatment. The evaluation may involve overnight monitoring of your breathing and other body functions as you sleep. Tests to detect obstructive sleep apnoea include:
Polysomnography. During this sleep study, you’re hooked up to equipment that monitors your heart, lung and brain activity, breathing patterns, arm and leg movements, and blood oxygen levels while you sleep. You may have a full-night study, in which you’re monitored all night, or a split-night sleep study.In a split-night sleep study, you’ll be monitored during the first half of the night. If you’re diagnosed with obstructive sleep apnoea, staff may wake you and give you continuous positive airway pressure for the second half of the night.This test can help your doctor diagnose obstructive sleep apnoea and adjust positive airway pressure therapy, if appropriate. This sleep study can also help rule out other sleep disorders, such as periodic limb movements of sleep or narcolepsy, which also can cause excessive daytime sleepiness, but require different treatment.
Home sleep apnoea testing. Under certain circumstances, your doctor may provide you with an at-home version of polysomnography to diagnose obstructive sleep apnoea. This test usually involves measurement of airflow, breathing patterns and blood oxygen levels, and possibly limb movements and snoring intensity.
Your doctor also may refer you to an ear, nose and throat doctor to rule out any anatomic blockage in your nose or throat.
Treatment
Lifestyle changes
For milder cases of obstructive sleep apnoea, your doctor may recommend lifestyle changes:
- Lose weight if you’re overweight.
- Exercise regularly.
- Drink alcohol moderately, if at all, and don’t drink several hours before bedtime.
- Quit smoking.
- Use a nasal decongestant or allergy medications.
- Don’t sleep on your back.
If these measures don’t improve your sleep or if your apnoea is moderate to severe, then your doctor may recommend other treatments. Certain devices can help open up a blocked airway. In other cases, surgery may be necessary.
Therapies
- Continuous positive airway pressure (CPAP)

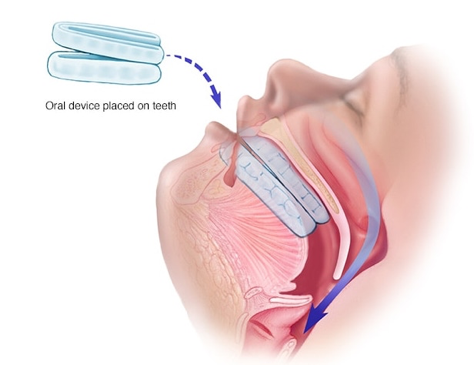
- Oral device
Positive airway pressure. If you have obstructive sleep apnea, you may benefit from positive airway pressure. In this treatment, a machine delivers air pressure through a piece that fits into your nose or is placed over your nose and mouth while you sleep.Positive airway pressure reduces the number of respiratory events that occur as you sleep, reduces daytime sleepiness and improves your quality of life.The most common type is called continuous positive airway pressure, or CPAP (SEE-pap). With this treatment, the pressure of the air breathed is continuous, constant and somewhat greater than that of the surrounding air, which is just enough to keep your upper airway passages open. This air pressure prevents obstructive sleep apnoea and snoring.Although CPAP is the most consistently successful and most commonly used method of treating obstructive sleep apnoea, some people find the mask cumbersome, uncomfortable or loud. However, newer machines are smaller and less noisy than older machines.Also, with some practice, most people learn to adjust the mask to obtain a comfortable and secure fit. You may need to try different types to find a suitable mask. Several options are available, such as nasal masks, nasal pillows or face masks.If you’re having particular difficulties tolerating pressure, some machines have special adaptive pressure functions to improve comfort. You also may benefit from using a humidifier along with your CPAP system.CPAP may be given at a continuous (fixed) pressure or varied (autotitrating) pressure. In fixed CPAP, the pressure stays constant. In autotitrating CPAP, the levels of pressure are adjusted if the device senses increased airway resistance.Bilevel positive airway pressure (BiPAP), another type of positive airway pressure, delivers a preset amount of pressure when you breathe in and a different amount of pressure when you breathe out.CPAP is more commonly used because it’s been well-studied for obstructive sleep apnoea and has been shown to effectively treat obstructive sleep apnoea. However, for people who have difficulty tolerating fixed CPAP, BiPAP or autotitrating CPAP may be worth a try.Don’t stop using your positive airway pressure machine if you have problems. Check with your doctor to see what adjustments you can make to improve its comfort. In addition, contact your doctor if you still snore despite treatment, if you begin snoring again or if your weight changes.
Mouthpiece (oral device). Though positive airway pressure is often an effective treatment, oral appliances are an alternative for some people with mild or moderate obstructive sleep apnoea. These devices may reduce your sleepiness and improve your quality of life.These devices are designed to keep your throat open. Some devices keep your airway open by bringing your jaw forward, which can sometimes relieve snoring and obstructive sleep apnoea. Other devices hold your tongue in a different position.If you and your doctor decide to explore this option, you’ll need to see a dentist experienced in dental sleep medicine appliances for the fitting and follow-up therapy. A number of devices are available. Close follow-up is needed to ensure successful treatment.
Surgery or other procedures
Surgery is usually considered only if other therapies haven’t been effective or haven’t been appropriate options for you. Surgical options may include:
- Surgical removal of tissue. Uvulopalatopharyngoplasty (UPPP) is a procedure in which your doctor removes tissue from the back of your mouth and top of your throat. Your tonsils and adenoids may be removed as well. UPPP usually is performed in a hospital and requires a general anesthetic.Doctors sometimes remove tissue from the back of the throat with a laser (laser-assisted uvulopalatoplasty) or with radiofrequency energy (radiofrequency ablation) to treat snoring. These procedures don’t treat obstructive sleep apnea, but they may reduce snoring.
- Upper airway stimulation. This new device is approved for use in people with moderate to severe obstructive sleep apnoea who can’t tolerate CPAP or BiPAP. A small, thin impulse generator is implanted under the skin in the upper chest. The device detects your breathing patterns and when necessary, stimulates the nerve that controls movement of the tongue.A study on the device found that it led to significant improvement in obstructive sleep apnoea symptoms and improvements in quality of life.
- Jaw surgery. In this procedure, called maxillomandibular advancement, the upper and lower parts of your jaw are moved forward from the rest of your facial bones. This enlarges the space behind the tongue and soft palate, making obstruction less likely.
- Surgical opening in the neck. You may need this form of surgery if other treatments have failed and you have severe, life-threatening obstructive sleep apnoea.In this procedure, called a tracheostomy, your surgeon makes an opening in your neck and inserts a metal or plastic tube through which you breathe. Air passes in and out of your lungs, bypassing the blocked air passage in your throat.
- Implants. This minimally invasive treatment involves placement of three tiny polyester rods in the soft palate. These inserts stiffen and support the tissue of the soft palate and reduce upper airway collapse and snoring. This treatment is recommended only for people with mild obstructive sleep apnoea.
- Other types of surgery may help reduce snoring and sleep apnoea by clearing or enlarging air passages, including:
- Nasal surgery to remove polyps or straighten a crooked partition between your nostrils (deviated septum)
- Surgery to remove enlarged tonsils or adenoids
Lifestyle and home remedies
In many cases, self-care may be the most appropriate way for you to deal with obstructive sleep apnoea. Try these tips:
- Lose weight. If you’re overweight or obese, even a slight loss of excess weight may help relieve constriction of your airway. Losing weight can also improve your health and quality of life, and may reduce your sleepiness during the day.
Exercise. Exercising, such as aerobic exercise and strength training, can help improve your condition. Aim to exercise about 150 minutes a week, and generally try to exercise most days of the week.
Avoid alcohol and medications such as tranquilizers and sleeping pills. Alcohol can worsen obstructive sleep apnoea and sleepiness and may lead to weight gain. Certain medications also can worsen your sleep.
Sleep on your side or abdomen rather than on your back. Sleeping on your back can cause your tongue and soft palate to rest against the back of your throat and block your airway. To prevent sleeping on your back, try sewing a tennis ball in the back of your pajama top.
Keep your nasal passages open while you sleep. If you have congestion, use a saline nasal spray to help keep your nasal passages open. Talk to your doctor about using nasal decongestants or antihistamines, because some medications may only be recommended for short-term use.
For obstructive sleep apnoea, some basic questions to ask your doctor include:
- What’s the most likely cause of my symptoms?
- Is my condition likely temporary or long lasting?
- What kinds of tests do I need? Do I need to go to a sleep clinic?
- What treatments are available and which do you recommend for me?
- I have other health conditions. How can I best manage these conditions together? Don’t hesitate to ask other questions that occur to you during your appointment.
Acute Tonsillitis

Tonsillitis is inflammation of the tonsils, two oval-shaped pads of tissue at the back of the throat — one tonsil on each side. Signs and symptoms of tonsillitis include swollen tonsils, sore throat, difficulty swallowing and tender lymph nodes on the sides of the neck.
Most cases of tonsillitis are caused by infection with a common virus, but bacterial infections also may cause tonsillitis. Because appropriate treatment for tonsillitis depends on the cause, it’s important to get a prompt and accurate diagnosis. Surgery to remove tonsils, once a common procedure to treat tonsillitis, is usually performed only when bacterial tonsillitis occurs frequently, doesn’t respond to other treatments or causes serious complications.
Symptoms
Tonsillitis most commonly affects children between preschool ages and the mid-teenage years. Common signs and symptoms of tonsillitis include:
- Red, swollen tonsils
- White or yellow coating or patches on the tonsils
- Sore throat
- Difficult or painful swallowing
- Fever
- Enlarged, tender glands (lymph nodes) in the neck
- A scratchy, muffled or throaty voice
- Bad breath
- Stomachache, particularly in younger children
- Stiff neck
- Headache
In young children who are unable to describe how they feel, signs of tonsillitis may include:
- Drooling due to difficult or painful swallowing
- Refusal to eat
- Unusual fussiness
When to see a doctor
It’s important to get an accurate diagnosis if your child has symptoms that may indicate tonsillitis. Call your doctor if your child is experiencing:
- A sore throat that doesn’t go away within 24 to 48 hours
- Painful or difficult swallowing
- Extreme weakness, fatigue or fussiness
Get immediate care if your child has any of these symptoms:
- Difficulty breathing
- Extreme difficulty swallowing
- Drooling
Causes
Tonsillitis is most often caused by common viruses, but bacterial infections can also be the cause.
The most common bacterium causing tonsillitis is Streptococcus pyogenes (group A streptococcus), the bacterium that causes strep throat.
Other strains of strep and other bacteria also may cause tonsillitis.
Why do tonsils get infected?
The tonsils are the immune system’s first line of defense against bacteria and viruses that enter your mouth. This function may make the tonsils particularly vulnerable to infection and inflammation. However, the tonsil’s immune system function declines after puberty — a factor that may account for the rare cases of tonsillitis in adults.
Risk factors
Risk factors for tonsillitis include:
- Young age. Tonsillitis most often occurs in children, but rarely in those younger than age 2. Tonsillitis caused by bacteria is most common in children ages 5 to 15, while viral tonsillitis is more common in younger children.
- Frequent exposure to germs. School-age children are in close contact with their peers and frequently exposed to viruses or bacteria that can cause tonsillitis.
Complications
Inflammation or swelling of the tonsils from frequent or ongoing (chronic) tonsillitis can cause complications such as:
- Difficulty breathing
- Disrupted breathing during sleep (obstructive sleep apnea)
- Infection that spreads deep into surrounding tissue (tonsillar cellulitis)
- Infection that results in a collection of pus behind a tonsil (peritonsillar abscess)
Strep infection
If tonsillitis caused by group A streptococcus or another strain of streptococcal bacteria isn’t treated, or if antibiotic treatment is incomplete, your child has an increased risk of rare disorders such as:llection of pus behind a tonsil (peritonsillar abscess)
Strep infection
Rheumatic fever, an inflammatory disorder that affects the heart, joints and other tissues
- Poststreptococcal glomerulonephritis, an inflammatory disorder of the kidneys that results in inadequate removal of waste and excess fluids from blood
Prevention
The germs that cause viral and bacterial tonsillitis are contagious. Therefore, the best prevention is to practice good hygiene. Teach your child to:
Wash his or her hands thoroughly and frequently, especially after using the toilet and before eating
- Avoid sharing food, drinking glasses, water bottles or utensils
- Replace his or her toothbrush after being diagnosed with tonsillitis
To help your child prevent the spread of a bacterial or viral infection to others:
- Keep your child at home when he or she is ill
- Ask your doctor when it’s all right for your child to return to school
- Teach your child to cough or sneeze into a tissue or, when necessary, into his or her elbow
- Teach your child to wash his or her hands after sneezing or coughing
Diagnosis
Your child’s doctor will start with a physical exam that will include:
- Using a lighted instrument to look at your child’s throat and likely his or her ears and nose, which may also be sites of infection
- Checking for a rash known as scarlatina, which is associated with some cases of strep throat
- Gently feeling (palpating) your child’s neck to check for swollen glands (lymph nodes)
- Listening to his or her breathing with a stethoscope
- Checking for enlargement of the spleen (for consideration of mononucleosis, which also inflames the tonsils)
Throat swab
With this simple test, the doctor rubs a sterile swab over the back of your child’s throat to get a sample of secretions. The sample will be checked in the clinic or in a lab for streptococcal bacteria. Many clinics are equipped with a lab that can get a test result within a few minutes. However, a second more reliable test is usually sent out to a lab that can return results within 24 to 48 hours.
If the rapid in-clinic test comes back positive, then your child almost certainly has a bacterial infection. If the test comes back negative, then your child likely has a viral infection. Your doctor will wait, however, for the more reliable out-of-clinic lab test to determine the cause of the infection.
Complete blood cell count (CBC)
Your doctor may order a CBC with a small sample of your child’s blood. The result of this test, which can often be completed in a clinic, produces a count of the different types of blood cells. The profile of what’s elevated, what’s normal or what’s below normal can indicate whether an infection is more likely caused by a bacterial or viral agent. A CBC is not often needed to diagnose strep throat. However, if the strep throat lab test is negative, the CBC may be needed to help determine the cause of tonsillitis.
Treatment
At-home care
Whether tonsillitis is caused by a viral or bacterial infection, at-home care strategies can make your child more comfortable and promote better recovery.
If a virus is the expected cause of tonsillitis, these strategies are the only treatment. Your doctor won’t prescribe antibiotics.
Your child will likely be better within seven to 10 days.
At-home care strategies to use during the recovery time include the following:
- Encourage rest. Encourage your child to get plenty of sleep.
- Provide adequate fluids. Give your child plenty of water to keep his or her throat moist and prevent dehydration.
- Provide comforting foods and beverage. Warm liquids — broth, caffeine-free tea or warm water with honey — and cold treats like ice pops can soothe a sore throat.
- Prepare a saltwater gargle. If your child can gargle, a saltwater gargle of 1 teaspoon (5 milliliters) of table salt to 8 ounces (237 milliliters) of warm water can help soothe a sore throat. Have your child gargle the solution and then spit it out.
- Humidify the air. Use a cool-air humidifier to eliminate dry air that may further irritate a sore throat, or sit with your child for several minutes in a steamy bathroom.
- Offer lozenges. Children older than age 4 can suck on lozenges to relieve a sore throat.
- Avoid irritants. Keep your home free from cigarette smoke and cleaning products that can irritate the throat.
- Treat pain and fever. Talk to your doctor about using ibuprofen (Advil, Children’s Motrin, others) or acetaminophen (Tylenol, others) to minimize throat pain and control a fever. Low fevers without pain do not require treatment.
Except for certain diseases, children and teenagers should not take aspirin because when used to treat symptoms of cold or flu-like illnesses, it has been linked to Reye’s syndrome, a rare but potentially life-threatening condition.
Antibiotics
If tonsillitis is caused by a bacterial infection, your doctor will prescribe a course of antibiotics. Penicillin taken by mouth for 10 days is the most common antibiotic treatment prescribed for tonsillitis caused by group A streptococcus. If your child is allergic to penicillin, your doctor will prescribe an alternative antibiotic.
Your child must take the full course of antibiotics as prescribed even if the symptoms go away completely. Failure to take all of the medication as directed may result in the infection worsening or spreading to other parts of the body. Not completing the full course of antibiotics can, in particular, increase your child’s risk of rheumatic fever and serious kidney inflammation.
Talk to your doctor or pharmacist about what to do if you forget to give your child a dose.
Surgery
Surgery to remove tonsils (tonsillectomy) may be used to treat frequently recurring tonsillitis, chronic tonsillitis or bacterial tonsillitis that doesn’t respond to antibiotic treatment. Frequent tonsillitis is generally defined as:
More than three to four episodes in one year
A tonsillectomy may also be performed if tonsillitis results in difficult-to-manage complications, such as:
- Obstructive sleep apnea
- Breathing difficulty
- Swallowing difficulty, especially meats and other chunky foods
- An abscess that doesn’t improve with antibiotic treatment
Tonsillectomy is usually done as an outpatient procedure, unless your child is very young, has a complex medical condition or if complications arise during surgery. That means your child should be able to go home the day of the surgery. A complete recovery usually takes seven to 14 days.
Oral Sub-mucous Fibrosis

Oral Submucous Fibrosis (OSF) is an extremely discomforting oral condition that is marked by the development of painful lesions inside the mouth that refuse to go away on their own. Know all about the disease, including its possible causes, symptoms, diagnosis and treatment options.
ORAL SUBMUCOUS FIBROSIS DEFINITION
This is a highly potent and chronic pre-cancerous condition that affects various portions of the oral cavity as well as the pharynx. It causes progressive fibrosis of submucosal tissues and juxta-epithelial inflammatory reactions. This disease also leads to fibro-elastic changes in the lamina propria along with epithelial atrophy, which results in stiffness of the oral mucosa. It may become impossible to open to the mouth due to the extreme stiffness of the jaw.
The name of the condition has been derived from the words “oral” (mouth), “submucosal” (below the mucosa or mucus secreting membrane of mouth) and “fibrosis” (scarring and hardening).
ORAL SUBMUCOUS FIBROSIS INCIDENCE
The disorder can affect people from all over the world. However, its prevalence is higher in places like South Africa, South-East Asia sand Middle East. Both adults and children can develop the condition.
ORAL SUBMUCOUS FIBROSIS CLASSIFICATION
This condition is clinically categorized into three stages:
STAGE 1: STOMATITIS
In this stage, the mucous membrane of the mouth is inflamed.
STAGE 2: FIBROSIS
This is marked by the development of lesions in the mouth, oral mucosa blanching as well as circular and vertical palpable fibrous patches in and around the mouth. This gives a mottled appearance to the buccal mucosa.
STAGE 3: SEQUELAE OF OSF
It is identified by the presence of Leukoplakia and various speech and hearing difficulty. There is another group classification system for OSF apart from the above staging system. This second system was developed in the year 1995 by Khanna and Andrade for surgical treatment of trismus. As per this staging system, OSF can be categorized into:
GROUP I
It is the earliest stage of the disorder and does not include any limitations in opening the mouth. Patients having an interincisal distance above 35 mm are included in this group.
GROUP II
It refers to those OSF patients who have an interincisal distance between 26 and 36 mm.
GROUP III
It includes moderately advanced cases where the interincisal distance of the patients is from 15 to 26 mm. These patients have fibrotic bands on the soft palate while anterior pillars of the fauces are also present.
GROUP IVA
Patients in this group have severe trismus and their interincisal distance is less than 15 mm. Extensive fibrosis of the entire oral mucosa is also present.
GROUP IVB
In sufferers included in this group, the condition reaches an extremely advanced stage with the oral mucosa undergoing premalignant and malignant changes.
ORAL SUBMUCOUS FIBROSIS CAUSES
Hard chewable substances, mainly betel nuts or areca nuts (Areca catechu), have various substances that harm the oral mucosa and destroys its elasticity. Mouth fresheners containing betel nut may also irritate the mucosa if consumed in large amounts. Other causes of this disorder include:
- Consumption of excessive amounts of red chilies
- Nutritional deficiencies
- Extreme climatic conditions
- Immunological disorders
ORAL SUBMUCOUS FIBROSIS PATHOGENESIS
The change in oral mucosa may be triggered by a chronic exposure to chili, betel nuts and pepper as well as a deficiency of zinc and iron. The mucosa eventually becomes hypersensitive towards these irritants.
In many cases, this hypersensitivity results in juxta-epithelial inflammation which leads to an increase in the fibroblastic activity. This leads to the formation of collagen fiber in the lamina propria.
The collagen fibers are non-degradable, which results in reduced phagocytic activity.
ORAL SUBMUCOUS FIBROSIS SYMPTOMS
The initial stage of OSF is characterized by a leathery sensation in the mucosa along with visible fibrotic bands. In a more advanced stage, the mucosa loses its elasticity and becomes stiff and blanched. This condition is thought to arise in the back of the mouth and gradually spread towards the outer parts. Some of its clinical features include the following:
- Trismus or incapability of opening the mouth because of oral fibrosis
- Change of taste
- Dryness of mouth
- Earache
- Loss of hearing, due to stenosis of eustachian tubes
- Nasal intonation of the voice
- Recurrent ulceration
- Increased salivation
- Difficulty in swallowing solid foods (only in cases where the esophagus is affected)
- Difficulty in opening and moving the mouth for activities like eating, talking and blowing
- Reduced movement of soft palate
- Small tongue
- Shrinking of the uvula
- Stiffening and thinning of the lips
- Oral Submucous Fibrosis Prevention
OSF is a completely preventable disorder. Avoiding chewing betel nut as well as mouth fresheners containing this eatable significantly reduces the chances of developing OSF. One should also limit the amount of chilies consumed. Having plenty of chilies may damage the oral mucosa and lead to this disorder.
ORAL SUBMUCOUS FIBROSIS DIAGNOSIS
OSF is generally diagnosed by studying the signs and symptoms exhibited by the patient. Doctors thoroughly study the medical history of patients and ask whether they have chewed betel nut or any similar substance. No laboratory tests can confirm the presence of this pre-cancerous condition. However, some recent researches show that OSF patients are likely to have decreased hemoglobin, iron, protein and vitamin B complex levels in the blood. The erythrocyte sedimentation rate is also believed to increase in these patients. At present, modern diagnostic tools like ultrasonography and x-ray are being used for detection of this disorder.
ORAL SUBMUCOUS FIBROSIS DIFFERENTIAL DIAGNOSIS
During a differential diagnosis, physicians should rule out the presence of the following conditions that are characterized by symptoms similar to OSF:
- Lichen Planus
- Squamous Cell Carcinoma
- Scleroderma
ORAL SUBMUCOUS FIBROSIS TREATMENT AND MANAGEMENTA biopsy screening of the patient is always performed before the treatment begins. The basic and most important guidelines to follow during treatment are:
- Refraining from chewing betel nuts and tobacco
- Eating less amounts of spicy foods
- Eating less chili
- Maintaining oral hygiene
- Following a diet that contains plenty of iron, vitamins A, B complex as well as C rich foods
- A doctor generally prescribes hydrocortisone (Efcorlin) in the form of chewable pallets. Patients have to chew one pallet every 3-4 hours every day for 3 to 4 weeks. Administering kenacort injection has also proved to be useful in curing OSF.
- In severe cases of the disorder, hydrocortisone 100 mg injection is administered into the submucosal area once or twice every day. The injection helps to relieve the symptoms and is continued for 2 to 3 weeks depending on the individual requirements. Two to three milliliter of Placentrax (human chorionic gonadotrophins) can also be administered through submucosal injection 2-3 times a week for 3 to 4 weeks. Routine management of OSF involves an additional Pentoxifylline (Trental) therapy. It is a methylxanthine derivative with vasodilating properties which can increase the mucosal vascularity.
- Regular exercise of the mouth helps to improve its range of opening. Thus, Physiotherapy can be useful in the management of OSF.
ORAL SUBMUCOUS FIBROSIS SURGICAL TREATMENT
Surgery may be required if the Fibrosis continues to progress despite all the above treatments and the interincisal distance gets below 2 cm. Various surgical treatment options adopted for remedying this condition include simple excision of fibrous bands and creating lingual pedicle and nasolabial flaps.
ORAL SUBMUCOUS FIBROSIS LASER TREATMENT
It is a latest treatment option used for curing OSF. According to a recent study, KTP-532 laser release process has been successful in increasing the opening range of the mouth in several patients over a twelve month follow up period.
ORAL SUBMUCOUS FIBROSIS STEM CELL THERAPY
Recent researches have proved the effectiveness and safety of intra-lesional injection of the autologous stem cells of bone marrow for treating OSF. Studies show that this injection stimulates angiogenesis in the affected area, which reduces the degree of Fibrosis. This significantly increases the opening range of the mouth.
ORAL SUBMUCOUS FIBROSIS PROGNOSIS
With the use of proper treatment, the prognosis or outcome of the disorder is positive in most patients. OSF can be cured completely when treated at an early stage.
Swollen Lymph Nodes in Neck
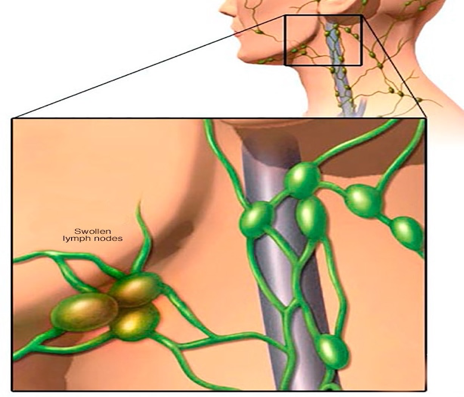
Swollen lymph nodes usually occur as a result of exposure to bacteria or viruses. When swollen lymph nodes are caused by an infection, this is known as lymphadenitis (lim-fad-uh-NIE-tis). Rarely, swollen lymph nodes are caused by cancer.
Your lymph nodes, also called lymph glands, play a vital role in your body’s ability to fight off infections. They function as filters, trapping viruses, bacteria and other causes of illnesses before they can infect other parts of your body. Common areas where you might notice swollen lymph nodes include your neck, under your chin, in your armpits and in your groin.
In some cases, the passage of time and warm compresses may be all you need to treat swollen lymph nodes. Treatment of lymphadenitis depends on the cause.
Symptoms
Your lymphatic system is a network of organs, vessels and lymph nodes situated throughout your body. Many lymph nodes are located in your head and neck region. Lymph nodes that frequently swell are in this area, as well as in your armpits and groin area.
Swollen lymph nodes are a sign that something is wrong somewhere in your body. When your lymph nodes first swell, you might notice:
- Tenderness and pain in the lymph nodes
- Swelling that may be the size of a pea or kidney bean, or even larger in the lymph nodes
- Depending on the cause of your swollen lymph nodes, other signs and symptoms you might have include:
- Runny nose, sore throat, fever and other indications of an upper respiratory infection
- General swelling of lymph nodes throughout your body — which may indicate an infection, such as HIV or mononucleosis, or an immune disorder, such as lupus or rheumatoid arthritis
- Hard, fixed, rapidly growing nodes, indicating a possible tumor
- Fever
- Night sweats
When to see a doctor
Some swollen lymph nodes return to normal when the underlying condition, such as a minor infection, gets better. See your doctor if you’re concerned or if your swollen lymph nodes:
- Have appeared for no apparent reason
- Continue to enlarge or have been present for two to four weeks
- Feel hard or rubbery, or don’t move when you push on them
- Are accompanied by persistent fever, night sweats or unexplained weight loss Seek immediate medical care if you’re having difficulty swallowing or breathing
Causes
Part of the immune system
A lymph node is a small, round or bean-shaped cluster of cells covered by a capsule of connective tissue. The cells are a combination of lymphocytes — which produce protein particles that capture invaders, such as viruses — and macrophages, which break down the captured material. Lymphocytes and macrophages filter your lymphatic fluid as it travels through your body and protect you by destroying invaders. Lymph nodes are located in groups, and each group drains a specific area of your body. You may be more likely to notice swelling in certain areas, such as in the lymph nodes in your neck, under your chin, in your armpits and in your groin. The site of the swollen lymph nodes may help identify the underlying cause.
The most common cause of swollen lymph nodes is an infection, particularly a viral infection, such as the common cold. Other possible causes of swollen lymph nodes include:
Common infections
- Strep throat
- Tuberculosis
- Measles
- Ear infections
- Infected (abscessed) tooth
- Mononucleosis
- Skin or wound infections, such as cellulitis
- Human immunodeficiency virus (HIV) — the virus that causes AIDS
Uncommon infections
- Certain sexually transmitted infections, such as syphilis
- Toxoplasmosis — a parasitic infection resulting from contact with the feces of an infected cat or eating undercooked meat
- Cat scratch fever — a bacterial infection from a cat scratch or bite
Immune system disorders
Lupus — a chronic inflammatory disease that can target your joints, skin, kidneys, blood cells, heart and lungs
Rheumatoid arthritis — a chronic inflammatory disease that targets the tissue that lines your joints (synovium)
Cancers
Lymphoma — cancer that originates in your lymphatic system
Leukemia — cancer of your body’s blood-forming tissue, including your bone marrow and lymphatic system
Other cancers that have spread (metastasized ) to lymph nodes
Other possible but rare causes include certain medications, such as the anti-seizure medication phenytoin (Dilantin) and preventive medications for malaria.
Complications
If infection is the cause of your swollen lymph nodes and isn’t treated, these complications might occur:
• Abscess formation. An abscess is a localized collection of pus caused by an infection. Pus contains fluid, white blood cells, dead tissue and bacteria or other invaders. An abscess may require drainage and antibiotic treatment. Bloodstream infection (bacteremia). A bacterial infection anywhere in your body can progress to sepsis, which is an overwhelming infection of the bloodstream. Sepsis may progress to organ failure and death. Treatment involves hospitalization and intravenous antibiotics.
Diagnosis
To diagnose what might be causing your swollen lymph nodes, your doctor may need:
- Your medical history. In addition, your doctor will want to know when and how your swollen lymph nodes developed and if you have any other signs or symptoms.
- A physical exam. Your doctor will also want to check lymph nodes near the surface of your skin for size, tenderness, warmth and texture. The site of your swollen lymph nodes and your other signs and symptoms will offer clues to the underlying cause.
- Blood tests. Depending on what your doctor suspects is causing your swollen lymph nodes, certain blood tests may be done to confirm or exclude the suspected underlying condition. The specific tests will depend on the suspected cause, but most likely will include a complete blood count (CBC). This helps evaluate your overall health and detect a range of disorders, including infections and leukemia.
- Imaging studies. A chest X-ray or computerized tomography (CT) scan of the affected area may help determine potential sources of infection or find tumors.
- Lymph node biopsy. Your doctor may have you undergo a biopsy. He or she will remove a sample from a lymph node or even an entire lymph node for microscopic examination.
Treatment
Swollen lymph nodes caused by a virus may return to normal after the viral infection resolves. Antibiotics are not useful to treat viral infections. Treatment for swollen lymph nodes from other causes depends on the cause:
- Infection. The most common treatment for swollen lymph nodes caused by a bacterial infection is antibiotics. If your swollen lymph nodes are due to an HIV infection, you’ll receive specific treatment for that condition.
- Immune disorder. If your swollen lymph nodes are a result of certain conditions, such as lupus or rheumatoid arthritis, treatment is directed at the underlying condition.
- Cancer. Swollen nodes caused by cancer require treatment for the cancer. Depending on the type of cancer, treatment may involve surgery, radiation or chemotherapy.
Lifestyle and home remedies
If your swollen lymph nodes are tender or painful, you might get some relief by doing the following:
- Apply a warm compress. Apply a warm, wet compress, such as a washcloth dipped in hot water and wrung out, to the affected area.
- Take an over-the-counter pain reliever. These include aspirin, ibuprofen (Advil, Motrin, others), naproxen (Aleve) or acetaminophen (Tylenol, others). Use caution when giving aspirin to children or teenagers. Though aspirin is approved for use in children older than age 2, children and teenagers recovering from chickenpox or flu-like symptoms should never take aspirin. Talk to your doctor if you have concerns.
- Get adequate rest. You often need rest to aid your recovery from the underlying condition. Preparing for your appointment
If you have swollen lymph nodes, you’re likely to start by first seeing your family doctor. When you call to set up your appointment, you may be urged to seek immediate medical care if you’re experiencing severe symptoms such as difficulty breathing or swallowing. Here’s some information to help you get ready for your appointment.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, ask if you need to do anything in advance.
- List any symptoms you’ve been experiencing, and for how long. Among other symptoms, your doctor will want to know if you’ve had flu-like symptoms, such as a fever or sore throat, and may ask whether you’ve noticed changes in your weight. Include on your list every symptom, from mild to severe, that you’ve noticed since your lymph nodes began to swell.
- Make a list of all recent exposures to possible sources of infection. These may include travel abroad, hiking in areas known to have ticks, eating undercooked meat, being scratched by a cat, or engaging in high-risk sexual behavior or sex with a new partner.
- Make a list of your key medical information, including other conditions you’re being treated for and the names of the medications that you’re taking. Include every prescription and over-the-counter (OTC) drug you use, as well as any vitamins and supplements.
- List questions to ask your doctor.
Swollen Lymph Nodes in Neck
Swollen lymph nodes usually occur as a result of exposure to bacteria or viruses. When swollen lymph nodes are caused by an infection, this is known as lymphadenitis (lim-fad-uh-NIE-tis). Rarely, swollen lymph nodes are caused by cancer.
Your lymph nodes, also called lymph glands, play a vital role in your body’s ability to fight off infections. They function as filters, trapping viruses, bacteria and other causes of illnesses before they can infect other parts of your body. Common areas where you might notice swollen lymph nodes include your neck, under your chin, in your armpits and in your groin.
In some cases, the passage of time and warm compresses may be all you need to treat swollen lymph nodes. Treatment of lymphadenitis depends on the cause.
Symptoms
Your lymphatic system is a network of organs, vessels and lymph nodes situated throughout your body. Many lymph nodes are located in your head and neck region. Lymph nodes that frequently swell are in this area, as well as in your armpits and groin area.
Swollen lymph nodes are a sign that something is wrong somewhere in your body. When your lymph nodes first swell, you might notice:
- Tenderness and pain in the lymph nodes
- Swelling that may be the size of a pea or kidney bean, or even larger in the lymph nodes
- Depending on the cause of your swollen lymph nodes, other signs and symptoms you might have include:
- Runny nose, sore throat, fever and other indications of an upper respiratory infection
- General swelling of lymph nodes throughout your body — which may indicate an infection, such as HIV or mononucleosis, or an immune disorder, such as lupus or rheumatoid arthritis
- Hard, fixed, rapidly growing nodes, indicating a possible tumor
- Fever
- Night sweats
When to see a doctor
Some swollen lymph nodes return to normal when the underlying condition, such as a minor infection, gets better. See your doctor if you’re concerned or if your swollen lymph nodes:
- Have appeared for no apparent reason
- Continue to enlarge or have been present for two to four weeks
- Feel hard or rubbery, or don’t move when you push on them
- Are accompanied by persistent fever, night sweats or unexplained weight loss Seek immediate medical care if you’re having difficulty swallowing or breathing
Causes
Part of the immune system
A lymph node is a small, round or bean-shaped cluster of cells covered by a capsule of connective tissue. The cells are a combination of lymphocytes — which produce protein particles that capture invaders, such as viruses — and macrophages, which break down the captured material. Lymphocytes and macrophages filter your lymphatic fluid as it travels through your body and protect you by destroying invaders. Lymph nodes are located in groups, and each group drains a specific area of your body. You may be more likely to notice swelling in certain areas, such as in the lymph nodes in your neck, under your chin, in your armpits and in your groin. The site of the swollen lymph nodes may help identify the underlying cause.
The most common cause of swollen lymph nodes is an infection, particularly a viral infection, such as the common cold. Other possible causes of swollen lymph nodes include:
Common infections
- Strep throat
- Tuberculosis
- Measles
- Ear infections
- Infected (abscessed) tooth
- Mononucleosis
- Skin or wound infections, such as cellulitis
- Human immunodeficiency virus (HIV) — the virus that causes AIDS
Uncommon infections
- Certain sexually transmitted infections, such as syphilis
- Toxoplasmosis — a parasitic infection resulting from contact with the feces of an infected cat or eating undercooked meat
- Cat scratch fever — a bacterial infection from a cat scratch or bite
Immune system disorders
Lupus — a chronic inflammatory disease that can target your joints, skin, kidneys, blood cells, heart and lungs
Rheumatoid arthritis — a chronic inflammatory disease that targets the tissue that lines your joints (synovium)
Cancers
Lymphoma — cancer that originates in your lymphatic system
Leukemia — cancer of your body’s blood-forming tissue, including your bone marrow and lymphatic system
Other cancers that have spread (metastasized ) to lymph nodes
Other possible but rare causes include certain medications, such as the anti-seizure medication phenytoin (Dilantin) and preventive medications for malaria.
Complications
If infection is the cause of your swollen lymph nodes and isn’t treated, these complications might occur:
• Abscess formation. An abscess is a localized collection of pus caused by an infection. Pus contains fluid, white blood cells, dead tissue and bacteria or other invaders. An abscess may require drainage and antibiotic treatment. Bloodstream infection (bacteremia). A bacterial infection anywhere in your body can progress to sepsis, which is an overwhelming infection of the bloodstream. Sepsis may progress to organ failure and death. Treatment involves hospitalization and intravenous antibiotics.
Diagnosis
To diagnose what might be causing your swollen lymph nodes, your doctor may need:
- Your medical history. In addition, your doctor will want to know when and how your swollen lymph nodes developed and if you have any other signs or symptoms.
- A physical exam. Your doctor will also want to check lymph nodes near the surface of your skin for size, tenderness, warmth and texture. The site of your swollen lymph nodes and your other signs and symptoms will offer clues to the underlying cause.
- Blood tests. Depending on what your doctor suspects is causing your swollen lymph nodes, certain blood tests may be done to confirm or exclude the suspected underlying condition. The specific tests will depend on the suspected cause, but most likely will include a complete blood count (CBC). This helps evaluate your overall health and detect a range of disorders, including infections and leukemia.
- Imaging studies. A chest X-ray or computerized tomography (CT) scan of the affected area may help determine potential sources of infection or find tumors.
- Lymph node biopsy. Your doctor may have you undergo a biopsy. He or she will remove a sample from a lymph node or even an entire lymph node for microscopic examination.
Treatment
Swollen lymph nodes caused by a virus may return to normal after the viral infection resolves. Antibiotics are not useful to treat viral infections. Treatment for swollen lymph nodes from other causes depends on the cause:
- Infection. The most common treatment for swollen lymph nodes caused by a bacterial infection is antibiotics. If your swollen lymph nodes are due to an HIV infection, you’ll receive specific treatment for that condition.
- Immune disorder. If your swollen lymph nodes are a result of certain conditions, such as lupus or rheumatoid arthritis, treatment is directed at the underlying condition.
- Cancer. Swollen nodes caused by cancer require treatment for the cancer. Depending on the type of cancer, treatment may involve surgery, radiation or chemotherapy.
Lifestyle and home remedies
If your swollen lymph nodes are tender or painful, you might get some relief by doing the following:
- Apply a warm compress. Apply a warm, wet compress, such as a washcloth dipped in hot water and wrung out, to the affected area.
- Take an over-the-counter pain reliever. These include aspirin, ibuprofen (Advil, Motrin, others), naproxen (Aleve) or acetaminophen (Tylenol, others). Use caution when giving aspirin to children or teenagers. Though aspirin is approved for use in children older than age 2, children and teenagers recovering from chickenpox or flu-like symptoms should never take aspirin. Talk to your doctor if you have concerns.
- Get adequate rest. You often need rest to aid your recovery from the underlying condition. Preparing for your appointment
If you have swollen lymph nodes, you’re likely to start by first seeing your family doctor. When you call to set up your appointment, you may be urged to seek immediate medical care if you’re experiencing severe symptoms such as difficulty breathing or swallowing. Here’s some information to help you get ready for your appointment.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, ask if you need to do anything in advance.
- List any symptoms you’ve been experiencing, and for how long. Among other symptoms, your doctor will want to know if you’ve had flu-like symptoms, such as a fever or sore throat, and may ask whether you’ve noticed changes in your weight. Include on your list every symptom, from mild to severe, that you’ve noticed since your lymph nodes began to swell.
- Make a list of all recent exposures to possible sources of infection. These may include travel abroad, hiking in areas known to have ticks, eating undercooked meat, being scratched by a cat, or engaging in high-risk sexual behavior or sex with a new partner.
- Make a list of your key medical information, including other conditions you’re being treated for and the names of the medications that you’re taking. Include every prescription and over-the-counter (OTC) drug you use, as well as any vitamins and supplements.
- List questions to ask your doctor.
Swollen Lymph Nodes in Neck
Swollen lymph nodes usually occur as a result of exposure to bacteria or viruses. When swollen lymph nodes are caused by an infection, this is known as lymphadenitis (lim-fad-uh-NIE-tis). Rarely, swollen lymph nodes are caused by cancer.
Your lymph nodes, also called lymph glands, play a vital role in your body’s ability to fight off infections. They function as filters, trapping viruses, bacteria and other causes of illnesses before they can infect other parts of your body. Common areas where you might notice swollen lymph nodes include your neck, under your chin, in your armpits and in your groin.
In some cases, the passage of time and warm compresses may be all you need to treat swollen lymph nodes. Treatment of lymphadenitis depends on the cause.
Symptoms
Your lymphatic system is a network of organs, vessels and lymph nodes situated throughout your body. Many lymph nodes are located in your head and neck region. Lymph nodes that frequently swell are in this area, as well as in your armpits and groin area.
Swollen lymph nodes are a sign that something is wrong somewhere in your body. When your lymph nodes first swell, you might notice:
- Tenderness and pain in the lymph nodes
- Swelling that may be the size of a pea or kidney bean, or even larger in the lymph nodes
- Depending on the cause of your swollen lymph nodes, other signs and symptoms you might have include:
- Runny nose, sore throat, fever and other indications of an upper respiratory infection
- General swelling of lymph nodes throughout your body — which may indicate an infection, such as HIV or mononucleosis, or an immune disorder, such as lupus or rheumatoid arthritis
- Hard, fixed, rapidly growing nodes, indicating a possible tumor
- Fever
- Night sweats
When to see a doctor
Some swollen lymph nodes return to normal when the underlying condition, such as a minor infection, gets better. See your doctor if you’re concerned or if your swollen lymph nodes:
- Have appeared for no apparent reason
- Continue to enlarge or have been present for two to four weeks
- Feel hard or rubbery, or don’t move when you push on them
- Are accompanied by persistent fever, night sweats or unexplained weight loss Seek immediate medical care if you’re having difficulty swallowing or breathing
Causes
Part of the immune system
A lymph node is a small, round or bean-shaped cluster of cells covered by a capsule of connective tissue. The cells are a combination of lymphocytes — which produce protein particles that capture invaders, such as viruses — and macrophages, which break down the captured material. Lymphocytes and macrophages filter your lymphatic fluid as it travels through your body and protect you by destroying invaders. Lymph nodes are located in groups, and each group drains a specific area of your body. You may be more likely to notice swelling in certain areas, such as in the lymph nodes in your neck, under your chin, in your armpits and in your groin. The site of the swollen lymph nodes may help identify the underlying cause.
The most common cause of swollen lymph nodes is an infection, particularly a viral infection, such as the common cold. Other possible causes of swollen lymph nodes include:
Common infections
- Strep throat
- Tuberculosis
- Measles
- Ear infections
- Infected (abscessed) tooth
- Mononucleosis
- Skin or wound infections, such as cellulitis
- Human immunodeficiency virus (HIV) — the virus that causes AIDS
Uncommon infections
- Certain sexually transmitted infections, such as syphilis
- Toxoplasmosis — a parasitic infection resulting from contact with the feces of an infected cat or eating undercooked meat
- Cat scratch fever — a bacterial infection from a cat scratch or bite
Immune system disorders
Lupus — a chronic inflammatory disease that can target your joints, skin, kidneys, blood cells, heart and lungs
Rheumatoid arthritis — a chronic inflammatory disease that targets the tissue that lines your joints (synovium)
Cancers
Lymphoma — cancer that originates in your lymphatic system
Leukemia — cancer of your body’s blood-forming tissue, including your bone marrow and lymphatic system
Other cancers that have spread (metastasized ) to lymph nodes
Other possible but rare causes include certain medications, such as the anti-seizure medication phenytoin (Dilantin) and preventive medications for malaria.
Complications
If infection is the cause of your swollen lymph nodes and isn’t treated, these complications might occur:
• Abscess formation. An abscess is a localized collection of pus caused by an infection. Pus contains fluid, white blood cells, dead tissue and bacteria or other invaders. An abscess may require drainage and antibiotic treatment. Bloodstream infection (bacteremia). A bacterial infection anywhere in your body can progress to sepsis, which is an overwhelming infection of the bloodstream. Sepsis may progress to organ failure and death. Treatment involves hospitalization and intravenous antibiotics.
Diagnosis
To diagnose what might be causing your swollen lymph nodes, your doctor may need:
- Your medical history. In addition, your doctor will want to know when and how your swollen lymph nodes developed and if you have any other signs or symptoms.
- A physical exam. Your doctor will also want to check lymph nodes near the surface of your skin for size, tenderness, warmth and texture. The site of your swollen lymph nodes and your other signs and symptoms will offer clues to the underlying cause.
- Blood tests. Depending on what your doctor suspects is causing your swollen lymph nodes, certain blood tests may be done to confirm or exclude the suspected underlying condition. The specific tests will depend on the suspected cause, but most likely will include a complete blood count (CBC). This helps evaluate your overall health and detect a range of disorders, including infections and leukemia.
- Imaging studies. A chest X-ray or computerized tomography (CT) scan of the affected area may help determine potential sources of infection or find tumors.
- Lymph node biopsy. Your doctor may have you undergo a biopsy. He or she will remove a sample from a lymph node or even an entire lymph node for microscopic examination.
Treatment
Swollen lymph nodes caused by a virus may return to normal after the viral infection resolves. Antibiotics are not useful to treat viral infections. Treatment for swollen lymph nodes from other causes depends on the cause:
- Infection. The most common treatment for swollen lymph nodes caused by a bacterial infection is antibiotics. If your swollen lymph nodes are due to an HIV infection, you’ll receive specific treatment for that condition.
- Immune disorder. If your swollen lymph nodes are a result of certain conditions, such as lupus or rheumatoid arthritis, treatment is directed at the underlying condition.
- Cancer. Swollen nodes caused by cancer require treatment for the cancer. Depending on the type of cancer, treatment may involve surgery, radiation or chemotherapy.
Lifestyle and home remedies
If your swollen lymph nodes are tender or painful, you might get some relief by doing the following:
- Apply a warm compress. Apply a warm, wet compress, such as a washcloth dipped in hot water and wrung out, to the affected area.
- Take an over-the-counter pain reliever. These include aspirin, ibuprofen (Advil, Motrin, others), naproxen (Aleve) or acetaminophen (Tylenol, others). Use caution when giving aspirin to children or teenagers. Though aspirin is approved for use in children older than age 2, children and teenagers recovering from chickenpox or flu-like symptoms should never take aspirin. Talk to your doctor if you have concerns.
- Get adequate rest. You often need rest to aid your recovery from the underlying condition. Preparing for your appointment
If you have swollen lymph nodes, you’re likely to start by first seeing your family doctor. When you call to set up your appointment, you may be urged to seek immediate medical care if you’re experiencing severe symptoms such as difficulty breathing or swallowing. Here’s some information to help you get ready for your appointment.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, ask if you need to do anything in advance.
- List any symptoms you’ve been experiencing, and for how long. Among other symptoms, your doctor will want to know if you’ve had flu-like symptoms, such as a fever or sore throat, and may ask whether you’ve noticed changes in your weight. Include on your list every symptom, from mild to severe, that you’ve noticed since your lymph nodes began to swell.
- Make a list of all recent exposures to possible sources of infection. These may include travel abroad, hiking in areas known to have ticks, eating undercooked meat, being scratched by a cat, or engaging in high-risk sexual behavior or sex with a new partner.
- Make a list of your key medical information, including other conditions you’re being treated for and the names of the medications that you’re taking. Include every prescription and over-the-counter (OTC) drug you use, as well as any vitamins and supplements.
- List questions to ask your doctor.
